Key Takeaways (expand)
- Iron is an essential mineral needed for the metabolism of all living organisms.
- The adult human body contains about 4 grams of iron, mostly in the form of hemoglobin and myoglobin.
- In food, iron is present in one of two forms: as a component of heme (a hemoglobin precursor that contains an iron atom), or nonheme iron (the predominant form in plant foods and dairy).
- The bioavailability of heme iron is significantly higher than non-heme: only about 2 – 20% of nonheme iron is absorbed (although other components of the diet can increase this, like the presence of vitamin C)!
- Iron is essential for the functioning of a wide variety of proteins involved in oxygen transport and storage, electron transport, energy metabolism, oxygen sensing, and DNA replication and repair.
- Some iron-dependent proteins also act as antioxidants or beneficial pro-oxidants.
- Among the many iron-dependent proteins that exist, some of the most important are hemoglobin and myoglobin (which are vital for keeping tissues throughout the body oxygenated), iron-dependent cytochromes (which are essential for cellular energy production), and iron-dependent ribonucleotide reductases (which are needed for DNA replication and repair).
- Iron also plays a role in immune function: during times of infection, the body has iron-withholding defenses that help keep iron away from the pathogens that need it to survive!
- Iron homeostasis is regulated by a hormone called hepcidin, which helps reduce the absorption and bioavailability of iron in times of excess, and increases iron absorption and mobilization when body stores become too low.
- When too much free iron accumulates in the body (often due to inherited genetic conditions, such as hereditary hemochromatosis), it can lead to oxidative stress and cellular damage, eventually impacting organ function, increasing the risk of cancer and heart disease, and potentially becoming fatal.
- Even in the absence of iron overload disorders, excess iron intake has been linked with a higher risk of cardiovascular disease.
- Iron absorption and metabolism depends on adequate levels of several other nutrients, including vitamin A, copper, and zinc.
- Iron is needed for the development of the central nervous system, especially during childhood.
- During pregnancy, adequate iron helps promote healthy gestation and prevent some adverse outcomes, including preterm birth and low birth weight.
- Iron deficiency is the most common nutrient deficiency among humans, and when it progresses to clinical anemia, causes symptoms such as brittle nails, mouth sores, fatigue, heart palpitations, rapid breathing, rapid heart rate, difficulty swallowing, and impaired thyroid function.
- People at highest risk of iron deficiency are children, adolescents, pregnant people, menstruating individuals, people with inflammatory disorders, athletes, people with malabsorption disorders (like celiac disease or inflammatory bowel diseases), and vegans and vegetarians.
Table of Contents[Hide][Show]
Along with being abundant in the earth’s crust, iron is one of the most thoroughly studied minerals in nutritional science, and is essential for the metabolism of all living organisms. The adult human body contains about 4 grams of iron (mostly in the form of hemoglobin and myoglobin)! Chemists first discovered the presence of iron in blood in 1713, but it was being used for therapeutic purposes as far back as the Iron Age (from about 1200 to 1000 BCE)! The word iron is thought to come from the Proto-Germanic word isarnan, which roughly means “holy metal” or “powerful metal”—referring to the use of iron to make swords during in the Crusades. However, the Latin word for iron, ferrum, is the source of its atomic symbol (Fe), as well as iron-related words like ferritin (a protein that stores iron) and transferrin (a glycoprotein that binds to iron and transports it through the blood).
Iron is an essential part of hundreds of enzymes and proteins involved in oxygen transport, energy production, DNA synthesis, cellular growth, cellular replication, and more! It’s also needed for some vital functions like reproduction, healing, and immunity.
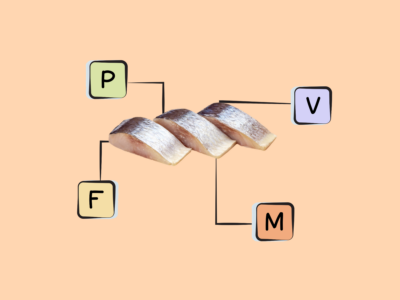
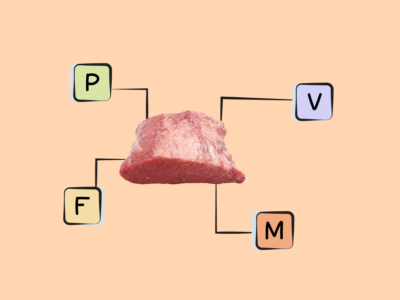
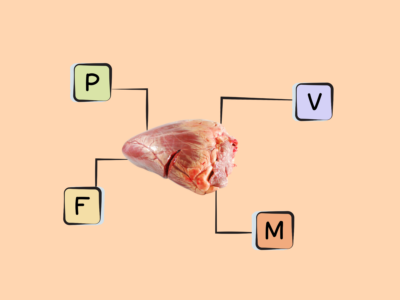
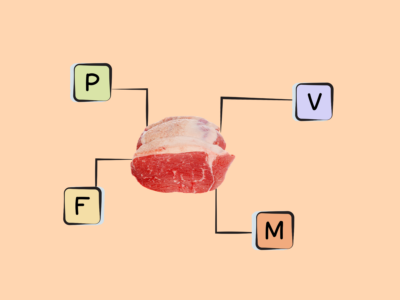
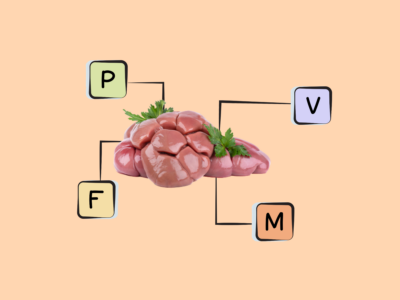
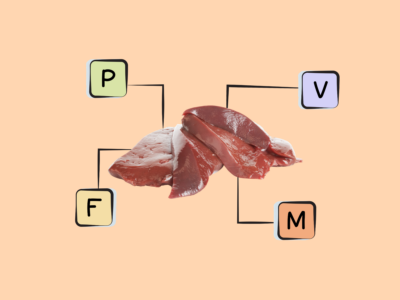
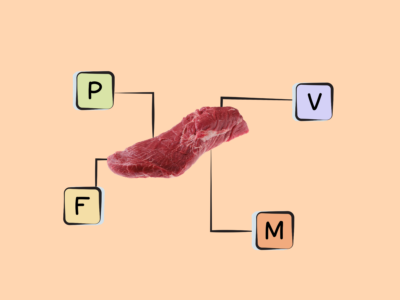
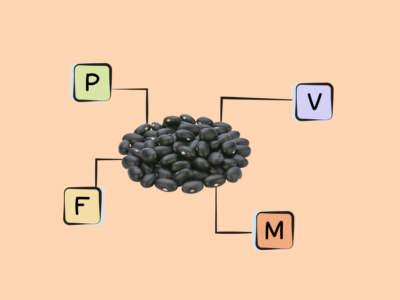
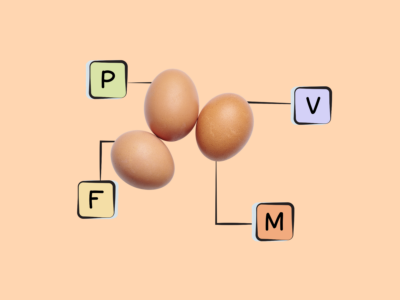
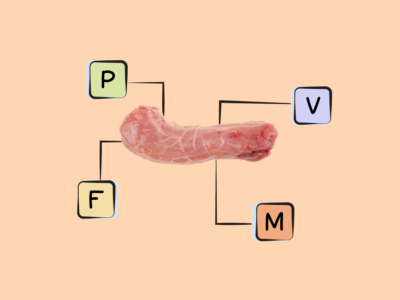
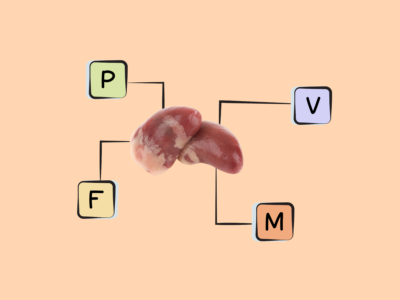
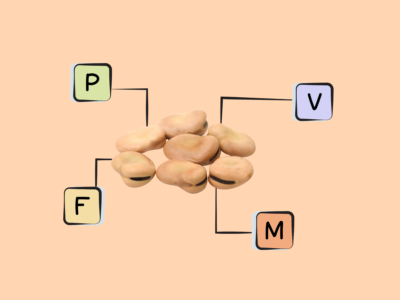
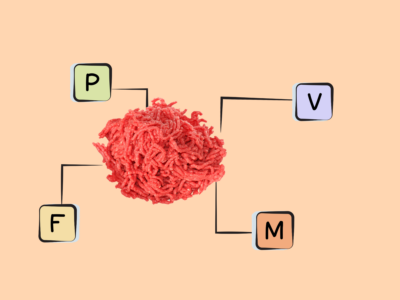
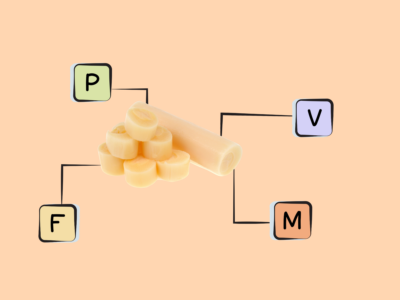
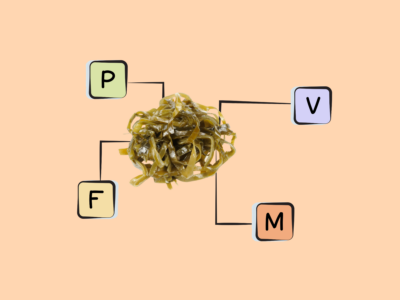
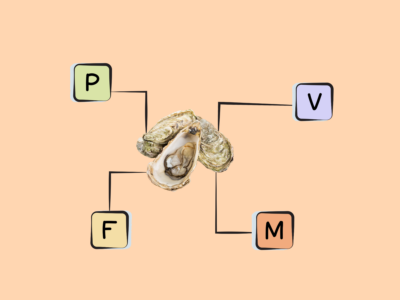
Food can contain one of two forms of iron: iron as a component of heme (a precursor to hemoglobin that’s composed of a ring-like organic compound with an iron atom attached) or nonheme iron (the predominant form in plant foods and dairy, although it’s also present in meat). Heme iron-rich foods include liver, red meat, and some shellfish (especially oysters, mussels, and clams). The best sources of iron in its non-heme form are dark leafy greens, legumes (such as lentils, kidney beans, peas, white beans, and chickpeas), and blackstrap molasses. And, some foods that normally have a low iron content are commercially fortified with iron, such as breakfast cereals, flour, and rice.
Ditch Diets. Embrace Nutrients. Start with this FREE Guide.
Sign up for the free Nutrivore Newsletter, your weekly, science-backed guide to improving health through nutrient-rich foods — without dieting harder —and get the Beginner’s Guide to Nutrivore delivered straight to your inbox!

What Are The Biological Roles of Iron?
Iron is essential for the functioning of a wide variety of proteins in the body—many (but not all!) of which have enzyme activity, and that are variously involved in oxygen transport and storage, electron transport, energy metabolism, oxygen sensing, DNA replication and repair, oxidation, and free radical scavenging. Some iron-dependent proteins even exhibit antioxidant or beneficial pro-oxidant functions.
On a technical level, these proteins fall into several distinct categories:
- iron-sulfur cluster proteins that help transfer electrons between molecules, and which are involved in DNA replication and repair (such as DNA polymerases and DNA helicases) or energy production (such as succinate dehydrogenase, aconitase, ferredoxin-1, isocitrate dehydrogenase, NADH dehydrogenase, and xanthine oxidase);
- heme enzymes involved in electron transfer (such as cytochrome c oxidase and cytochromes a, b, and f) or with oxidase activity (such as the cytochrome P450 family, sulfite oxidase, myeloperoxidase, catalase, peroxidases, cyclooxygenase, and endothelial nitric oxide synthase);
- nonheme enzymes that use iron as a cofactor (such as several amino acid hydroxylases and ribonucleotide reductase);
- nonheme proteins needed to transport and store iron (such as ferritin, transferrin, lactoferrin, hemopexin, and haptoglobin); and lastly,
- globin-heme proteins, which are nonenzymatic proteins needed to transport and store oxygen—including hemoglobin (the protein in red blood cells responsible for carrying oxygen from the lungs to every other cell in the body), myoglobin (an oxygen-binding protein in the muscles), and neuroglobin (a protein found in both peripheral and central nervous system neurons).
Although the number of iron-dependent proteins is huge, a handful are particularly noteworthy. For example, hemoglobin and myoglobin are vital for keeping tissues throughout the body oxygenated: hemoglobin contains four iron-containing heme molecules (it’s the iron itself that binds to oxygen!), and has a unique ability to rapidly acquire oxygen when it makes contact with the lungs—after which it releases the oxygen as needed throughout other tissues. Likewise, myoglobin (which contains one iron-containing heme molecule) helps coordinate the supply-and-demand delivery of oxygen to muscles as they work, ensuring muscle tissue stays oxygenated. Meanwhile, iron-dependent cytochromes serve as electron carriers during ATP synthesis, making them essential for cellular energy production (and therefore life itself!). Cytochrome P450 is a particularly important family of enzymes needed for detoxifying and metabolizing pollutants and drugs, as well as metabolizing many biological molecules (such as fatty acids, organic acids, sterols, steroids, prostaglandins, vitamin A, vitamin D, and vitamin K). Some heme-containing peroxidases and catalase are important for protecting cells against reactive oxygen species (ROS), due to their ability to catalyze the conversion of hydrogen peroxide into oxygen and water. And, iron-dependent ribonucleotide reductases are needed for the conversion of nucleotides to deoxynucleotides, making them essential for DNA replication and repair.
In addition to its protein and enzyme functions, iron plays an important role in immunity. Most pathogens require iron in order to grow and spread, and some immune cells (namely T lymphocytes) likewise need iron to differentiate and proliferate. During times of infection, the body up-regulates hepcidin synthesis so that blood concentrations of iron decrease while concentrations of ferritin (which stores iron) increase—effectively keeping iron away from the pathogens that need it to survive!
While adequate iron is essential for life, too much free iron in the body can lead to oxidative stress and cellular damage, which can eventually impact organ function and become fatal. What’s more, the body excretes relatively little iron under most circumstances, bringing the the potential for toxic levels of buildup (especially compared to micronutrients that are more readily eliminated, such as water-soluble vitamins). To compensate, the body has mechanisms in place for tightly regulating iron metabolism, helping avoid both deficiency and overload. In particular, a hormone called hepcidin serves as the master regulator for iron homeostasis: when iron stores are sufficient, this hormone helps reduce the absorption of dietary iron, decreases iron bioavailability, and promotes cellular iron sequestration; when iron stores are too low, hepcidin levels decrease so that iron absorption and mobilization can increase! The body is also able to conserve iron by recycling it: in the spleen, macrophages engulf aging red blood cells, recovering about 20 mg of iron each day from heme; the recovered iron is then deposited in ferritin or exported to transferrin (which carries iron in the blood) to be delivered to other tissues.
How Does Iron Interact with Other Nutrients?
Iron has a number of important interactions with other minerals and vitamins. For example, vitamin A deficiency can alter iron metabolism, potentially worsening iron-deficiency anemia; supplementing with vitamin A has been shown to improve iron status in children and pregnant women. And, that relationship may be a two-way street: rodent studies have shown that iron deficiency can likewise alter the level of vitamin A in the liver and blood.
Copper, too, is needed for iron metabolism and for the transport of iron from the liver to the bone marrow, where red blood cells are formed; in both animals and humans, copper deficiency can lead to iron accumulation in the liver and even cirrhosis (a late-stage liver disease characterized by permanent scarring). Meanwhile, high iron intakes have been shown to interfere with copper absorption, especially in infants.
Zinc deficiency can also exacerbate iron-deficiency anemia, while iron supplements can inhibit the absorption of supplemental zinc when taken together on an empty stomach (though this issue goes away if taken with food!). Calcium is known to block both heme and nonheme iron absorption from food and supplements—but the body appears to compensate for this by adjusting iron homeostasis, because most studies don’t show a significant negative impact of calcium intake on iron status. Studies have also shown that chromium and manganese can inhibit iron absorption due to shared absorptive pathways.
Importantly, when vitamin C is consumed alongside nonheme iron, it reduces the iron into its ferrous (Fe2+) form—creating a highly absorbable iron-ascorbic acid complex that makes the nonheme iron much more bioavailable!
Everything You Need to Jump into Nutrivore TODAY!
Nutrivore Quickstart Guide
The Nutrivore Quickstart Guide e-book explains why and how to eat a Nutrivore diet, introduces the Nutrivore Score, gives a comprehensive tour of the full range of essential and important nutrients!
Plus, you’ll find the Top 100 Nutrivore Score Foods, analysis of food groups, practical tips to increase the nutrient density of your diet, and look-up tables for the Nutrivore Score of over 700 foods.
Buy now for instant digital access.
How Does Iron Affect Health and Disease?
Because of its diverse functions in the body, iron plays an important part in preventing disease and maintaining overall health.
Iron and Development
Iron is needed for central nervous system development, especially during childhood: due to the role of iron-dependent enzymes in neurotransmitter synthesis, nerve myelination, and the energy metabolism of neurons, iron can ultimately help support healthy psychomotor and cognitive development.
Studies have found that in older children, adolescents, and women with iron deficiency, iron supplementation was able to improve concentration and attention, and potentially even boost some measures of IQ!
Iron and Pregnancy
In pregnant women, adequate iron is needed for healthy gestation and to prevent adverse pregnancy outcomes. Observational studies have linked severe anemia during pregnancy to preterm birth, low birth weight infants, and higher risk of mortality for both the mother and newborn. Iron requirements significantly increase during the second and third trimesters, in particular, due to the rising iron needs for the placenta and developing fetus—making it particularly important to have adequate dietary intake during this time. In fact, research has shown that nearly 30% of women in their third trimester of pregnancy are iron deficient!
Iron and Restless Leg Syndrome
Iron may also play a role in of restless leg syndrome (also called Willis-Ekbom disease), which is a neurological disorder characterized by an irresistible urge to move your legs. Although its cause isn’t fully understood, it appears to have a genetic component (it’s inherited in about 50% of sufferers), and iron may be involved through affecting the activity of tyrosine hydroxylase—an enzyme used for synthesizing the neurotransmitter dopamine. But, more research is needed to test whether iron supplementation can relieve symptoms of this condition.
Iron and Fatigue
Fatigue is a well-known symptom of iron deficiency anemia, but even in the absence of deficiency, iron may help improve fatigue! A 2018 systematic review of 18 randomized controlled trials found that among non-iron-deficient individuals, iron supplementation led to reductions in self-reported fatigue.
A 2023 double-blind, randomized, placebo-controlled, parallel-group trial of non-anemic athletes also found benefit from iron supplementation during exercise training. For participants in this study, four weeks of taking oral iron supplements (3.6 mg daily) led to significant decreases in subjective fatigue.
Not surprisingly, a number of studies have also shown that iron consumption helps improve fatigue in people with iron deficiency. A 2020 randomized controlled trial of iron-deficient blood donors found that 8 – 12 weeks of oral iron supplementation (in the form of 10 g iron fumarate) significantly improved participants’ fatigues, among other benefits (including sleep quality and headaches).
And, a 2012 randomized controlled trial of menstruating women with low ferritin levels, who also complained of fatigue, found that 12 weeks of iron supplementation (80 mg of elemental iron daily) significantly reduced the mean score on the Current and Past Psychological Scale for fatigue. Specifically, fatigue scores reduced by decreased by 47.7% in the iron group, compared to 28.8% in the placebo group.
Iron and Hypothyroidism
Iron plays a role in thyroid health, and may specifically help protect against hypothyroidism. For one, observational research shows a link between iron status and hypothyroidism risk. A 2016 cross-sectional analysis of Nepalese children found that compared to non-anemic and iron sufficient children, those with iron deficiency were almost twice as likely to have hypothyroidism, while those with anemia had a 5.5-fold greater risk of having hypothyroidism.
Similarly, a 2021 systematic review and meta-analysis of 636 studies found that iron deficiency in pregnant and reproductive-age women was associated with significantly higher risk of thyroid disorders. For pregnant women, iron deficiency increased the risk of overt hypothyroidism by 60% and subclinical hypothyroidism by 37%, while for women of reproductive age in general, iron deficiency increased the risk of positive thyroid peroxidase antibody (a marker of autoimmune thyroid disease) by 89%.
A 2023 systematic review and meta-analysis of 10 cross-sectional studies similarly found that iron deficiency significantly increases the prevalence of autoimmune thyroid markers (anti-thyroglobulin antibodies and anti-thyroid peroxidase antibodies), while also associating with lower thyroid hormone levels.
Iron and Hair Loss
Adequate iron intake may be important for protecting against various forms of hair loss, largely due to iron’s involvement in various physiologic processes within the hair follicle (as well as limiting the amount of oxygen that gets transported for hair growth). According to a 2013 retrospective case-control study, premenopausal women with female pattern hair loss were much more likely to have low serum ferritin levels, relative to sex- and age-matched controls. Likewise, 22.7% of men with male pattern hair loss had serum ferritin levels below 70 µg/L, whereas none of the age-matched male controls had serum ferritin in this range.
A 2022 systematic review and meta-analysis of 36 studies looked at iron deficiency in women and the prevalence of nonscarring alopecia (a category of hair loss including female pattern baldness, the autoimmune disease alopecia areata, excessive hair shedding called telogen effluvium, and several other less common conditions). The results showed that women with nonscarring alopecia had significantly lower ferritin values compared to women without this form of hair loss. And, a 2023 retrospective study found that female patients with hair loss related to iron insufficiency saw subjective improvement of hair regrowth following iron supplementation.
Iron and Migraine Headaches
Some research has linked iron to the occurrence of migraine headaches, especially among women. A 2019 case-control study found that compared to non-migraine controls, women who experience migraines had significantly lower levels of hemoglobin and serum ferritin levels, as well as higher rates of iron-deficiency anemia. A 2016 case-control study also found that iron deficiency was significantly associated with pure menstrual migraines (migraines occurring only around the first day of menstruation) and menstrually related migraines (migraines occurring at the beginning of menstruation, but potentially at other times of the cycle as well).
A 2021 cross-sectional study also found that for women aged 20 to 50, dietary iron intake was inversely associated with severe headaches and migraines, while for women over the age of 50, higher serum ferritin levels were protective against migraine occurrence. No significant relationship was seen for men!
Iron and Sleep Disorders
Iron may play a role in sleep disorders, including insomnia. A 2021 cross-sectional study and meta-analysis found that compared to non-anemic individuals, people with iron deficiency anemia were 32% more likely to have insomnia; after excluding people with chronic inflammation (C-reactive protein levels greater than 1 mg/L), the risk increase rose to 68%. And, the meta-analysis portion of this paper (including over 22,000 participants) found a similar association between anemia and insomnia, with anemia increasing the risk of insomnia by 39%.
A 2015 cross-sectional study of 104 patients with iron deficiency anemia and 80 non-anemic controls similarly found that iron deficiency was significantly associated with worse sleep quality. This link persisted even after adjusting for psychological symptoms such as depression and anxiety. A 2020 randomized controlled trial found that iron supplementation was able to significantly improve sleep quality among iron-deficient blood donors!
Didn’t know iron was this amazing? Maybe your friends will enjoy this too!
What Are the Symptoms of Iron Deficiency?
Iron deficiency is the most widespread nutrient deficiency in the world, affecting up to 2 billion people globally. Children, adolescents, frequent blood donors, and menstruating or pregnant individuals are at the highest risk of not getting enough iron (in fact, nearly one out of five pregnant people have been shown to be iron deficient!). But, iron deficiency can also occur from chronic blood loss, especially gastrointestinal tract bleeding (such as from parasite infection, peptic ulcers, gastrointestinal tumors, hiatal hernia, diverticulosis, chronic kidney disease, and even heavy endurance exercise). People with celiac disease, atrophic gastritis, or inflammatory bowel diseases can also develop iron deficiency due to impaired iron absorption. Vegetarians and vegans may also be more susceptible to iron deficiency due to the lower bioavailability of plant-based iron sources (by some estimates, the bioavailability of iron from vegetarian diets is about half that of an omnivorous diet, meaning the amount of iron needed from the diet may be higher than recommended intakes for omnivores). And, people with acute or chronic inflammation resulting from cancer, critical illness, chronic infection, or other inflammatory disorders can cause abnormally low levels of circulating iron, leading to anemia (when this occurs, it’s known as “anemia of chronic disease”).
Iron deficiency happens when the body’s iron reserves get depleted, leading to an inadequate supply of iron to cells. When those iron stores drop low enough so that hemoglobin synthesis and red blood cell formation are impaired, the result is microcytic anemia—a condition where red blood cells become small and pale in color, and can’t deliver adequate oxygen to tissues and organs. Anemia officially occurs when hemoglobin concentrations drop below two standard deviations of the mean for the average healthy population of the same age, gender, and altitude (the decreased oxygen levels in high-altitude air can affect iron metabolism!). Importantly, anemia can also result from vitamin B12 or folate deficiency, making it important to screen for these deficiencies as well.
Although there aren’t obvious symptoms during early-stage iron deficiency (when iron stores are low but the functional supply is still sufficient), as it progresses to anemia, iron deficiency can cause fatigue, heart palpitations, rapid heart rate, and rapid breathing. Because there’s less hemoglobin in red blood cells (impairing the delivery of oxygen to body tissues) and less myoglobin in muscle cells (impairing the delivery of oxygen to mitochondria for energy production), anemia can reduce athletic performance and physical work capacity. Additionally, iron deficiency can impair thyroid hormone synthesis and thyroid function, making it hard to maintain a normal body temperature and reducing resiliency to cold exposure. Studies have shown that iron deficiency is particularly detrimental for people with heart disease, including coronary artery disease, heart failure, and pulmonary hypertension.
Additional symptoms of iron deficiency include brittle or spoon-shaped nails, atrophied taste buds, sore tongue, sores at the corners of the mouth, and impaired immune function. In very severe cases of iron-deficiency anemia, the pharyngeal muscles in the esophagus can degrade, leading to the formation of webs of tissue (called Plummer-Vinson syndrome) that make swallowing difficult.
In children, iron deficiency (even when present without clinical anemia) is associated with impaired cognitive development, abnormal behavioral patterns, and poor achievement in school. In pregnant women, iron deficiency can reduce gestation length and lead to low body-weight newborns.
For most people, iron deficiency is assessed by measuring circulating iron levels, iron stores, and certain blood parameters—in particular, serum iron, total iron binding capacity, the iron-storage protein serum ferritin, soluble transferrin receptor, and saturation of transferrin. But, inflammation and infection can alter blood levels of ferritin, so measuring inflammatory markers (such as C-reactive protein or fibrinogen) is recommended while assessing iron status! And, due to a tendency for iron status to decline throughout pregnancy, pregnant women have different iron level cut-offs to determine deficiency.
Iron deficiency is often treated with dietary supplements, but it’s important to note that this can cause some unpleasant side effects—including stomach ache, gastrointestinal irritation, nausea, vomiting, constipation, or diarrhea. In order to prevent these symptoms, the tolerable upper intake level for iron is set at 45 mg per day for most adults. Iron supplements can also interfere with the absorption and effectiveness of some medications, including antibiotics, hypothyroid medications, Parkinson’s disease medications, histamine receptor antagonists, proton pump inhibitors, and anti-osteoporosis drugs.
Want to know the top 25 foods for this awesome nutrient?

The Top 25 Foods for Every Nutrient
The Top 25 Foods for Every Nutrient e-book is a well-organized, easy-to-use, grocery store-friendly guide to help you choose foods that fit your needs of 43 important nutrients while creating a balanced nutrient-dense diet.
Get two “Top 25” food lists for each nutrient, plus you’ll find RDA charts for everyone, informative visuals, fun facts, serving sizes and the 58 foods that are Nutrient Super Stars!
Buy now for instant digital access.
Why is it Bad to Have Too Much Iron?
While iron is essential for human health and life, too much can increase the risk of some serious health conditions—particularly for people with certain genetic or acquired diseases that affect iron metabolism. For example, a group of late-onset, autosomal recessive disorders called hereditary hemochromatosis can cause the body to absorb too much iron from food, causing iron to build up in the vital organs (including the liver and heart). Over time, iron overload can lead to liver cirrhosis, heart muscle damage (cardiomyopathy), hypogonadism, joint problems, and increased skin pigmentation, as well as an increased risk of liver cancer, neurodegenerative diseases, and type 2 diabetes (due to the oxidative stress associated with iron overload causing damage to pancreatic beta-cells and impairing insulin secretion).
People with hereditary hemochromatosis are advised to avoid alcohol (due to the increased risk of liver cirrhosis) and high-dose vitamin C supplementation (due to its iron absorption-enhancing abilities), and may require phlebotomy or chelation therapy to help remove excess iron from the body.
In addition to hereditary hemochromatosis, the genetic disorders hypotransferrinemia, aceruloplasminemia, porphyria cutanea tarda, and Friedreich’s ataxia can also cause excessive iron to accumulate—as can some acquired iron-overload diseases such as beta-thalassemia (an inherited blood disorder affecting hemoglobin production), sideroblastic anemia (a family of blood disorders where the bone marrow can’t properly use iron to make red blood cells), pyruvate kinase deficiency, and hemolytic anemia (a disorder where red blood cells get destroyed more rapidly than they can be replaced).
Even among people without iron-related genetic disorders, high iron intake (especially heme iron) has been linked with an increased risk of cardiovascular disease. One meta-analysis of prospective studies found that people with the highest versus lowest heme iron intake had a 31% greater chance of developing heart disease over time.
In addition, iron toxicity can happen acutely from accidental overdose (in fact, among children under the age of six, the leading cause of poisoning fatalities is overdose from iron-containing products). Acute toxicity can occur from ingesting iron doses of 20 to 60 mg per kilogram of body weight, leading to initial symptoms of nausea, vomiting, lethargy, low blood pressure, fever, weak and rapid pulse, tarry stools, breathing difficulties, and even coma. If the acute toxicity isn’t immediately fatal, various body systems can begin to fail within the 48 hours immediately following iron ingestion—including problems with the cardiovascular system, liver, kidney, blood, and/or central nervous system. Long-term damage can then develop in the central nervous system, stomach, or liver.
How Much Iron Do We Need?
The recommended dietary allowance (RDA) for iron is 18 mg per day for premenopausal women, 27 mg per day during pregnancy, 9 mg per day while breast-feeding, and 8 mg daily for men and postmenopausal women. Because vegetarian and vegan diets predominantly contain the less bioavailable type of iron (nonheme), it’s recommended that people who don’t eat meat aim for about 1.8 times the normal iron RDA.
It’s worth noting that iron as a component of heme is significantly more bioavailable than nonheme iron. In fact, only about 2 – 20% of nonheme iron is absorbed, although the actual amount depends on a variety of factors. For example, vitamin C strongly enhances nonheme absorption, as do fermented foods and alcohol. A peptide in meat—called the meat-fish-poultry-factor—enhances the absorption of any nonheme iron present in the meal, whether of plant or animal origin. Conversely, phytic acid (such as from grains, legumes, nuts, and seeds) and polyphenols (such as from tea and coffee) can bind to nonheme iron, forming insoluble complexes that can’t enter intestinal cells. And, while meat contains both heme and nonheme iron, its heme iron can get converted to nonheme during extended high-temperature cooking, reducing its bioavailability! That being said, once they’re taken into intestinal cells, heme and nonheme iron are treated the same way by the body.
| 0 – 6 months | |||||
| 6 months to < 12 months | |||||
| 1 yr – 3 yrs | |||||
| 4 yrs – 8 yrs | |||||
| 9 yrs – 13 yrs | |||||
| 14 yrs – 18 yrs | |||||
| 19 yrs – 50 yrs | |||||
| 51+ yrs | |||||
| Pregnant (14 – 18 yrs) | |||||
| Pregnant (19 – 30 yrs) | |||||
| Pregnant (31 – 50 yrs) | |||||
| Lactating (14 – 18 yrs) | |||||
| Lactating (19 – 30 yrs) | |||||
| Lactating (31 – 50 yrs) |
Nutrient Daily Values
Nutrition requirements and recommended nutrient intake for infants, children, adolescents, adults, mature adults, and pregnant and lactating individuals.
What Are the Best Food Sources of Iron?
The following foods have high concentrations of iron, containing at least 50% of the recommended dietary allowance per serving, making them our best food sources of this valuable mineral!
Want to know the top 500 most nutrient-dense foods?

Top 500 Nutrivore Foods
The Top 500 Nutrivore Foods e-book is an amazing reference deck of the top 500 most nutrient-dense foods according to their Nutrivore Score. Think of it as the go-to resource for a super-nerd, to learn more and better understand which foods stand out, and why!
If you are looking for a quick-reference guide to help enhance your diet with nutrients, and dive into the details of your favorite foods, this book is your one-stop-shop!
Buy now for instant digital access.
What Are Good Food Sources of Iron?
The following foods are also excellent or good sources of iron, containing at least 10% (and up to 50%) of the daily value per serving.
Nutrivore Is a Game-Changer—This FREE Guide Shows You Why
Sign up for the free Nutrivore Newsletter, your weekly, science-backed guide to improving health through nutrient-rich foods — without dieting harder —and get the Beginner’s Guide to Nutrivore delivered straight to your inbox!

Citations
Expand to see all scientific references for this article.
Anderson GJ, Darshan D, Wilkins SJ, Frazer DM. Regulation of systemic iron homeostasis: how the body responds to changes in iron demand. Biometals. 2007 Jun;20(3-4):665-74. doi: 10.1007/s10534-006-9030-2.
Ani M, Moshtaghie AA. The effect of chromium on parameters related to iron metabolism. Biol Trace Elem Res. 1992 Jan-Mar;32:57-64. doi: 10.1007/BF02784588.
Beard JL. Iron biology in immune function, muscle metabolism and neuronal functioning. J Nutr. 2001 Feb;131(2S-2):568S-579S; discussion 580S. doi: 10.1093/jn/131.2.568S.
Falkingham M, Abdelhamid A, Curtis P, Fairweather-Tait S, Dye L, Hooper L. The effects of oral iron supplementation on cognition in older children and adults: a systematic review and meta-analysis. Nutr J. 2010 Jan 25;9:4. doi: 10.1186/1475-2891-9-4.
Fleming MD. The regulation of hepcidin and its effects on systemic and cellular iron metabolism. Hematology Am Soc Hematol Educ Program. 2008:151-8. doi: 10.1182/asheducation-2008.1.151.
Garofalo V, Condorelli RA, Cannarella R, Aversa A, Calogero AE, La Vignera S. Relationship between Iron Deficiency and Thyroid Function: A Systematic Review and Meta-Analysis. Nutrients. 2023 Nov 15;15(22):4790. doi: 10.3390/nu15224790.
Gupta PM, Perrine CG, Mei Z, Scanlon KS. Iron, Anemia, and Iron Deficiency Anemia among Young Children in the United States. Nutrients. 2016 May 30;8(6):330. doi: 10.3390/nu8060330.
Gür-Özmen S, Karahan-Özcan R. Iron Deficiency Anemia Is Associated with Menstrual Migraine: A Case-Control Study. Pain Med. 2016 Mar;17(3):596-605. doi: 10.1093/pm/pnv029.
Hershko C, Skikne B. Pathogenesis and management of iron deficiency anemia: emerging role of celiac disease, helicobacter pylori, and autoimmune gastritis. Semin Hematol. 2009 Oct;46(4):339-50. doi: 10.1053/j.seminhematol.2009.06.002.
Hess SY. The impact of common micronutrient deficiencies on iodine and thyroid metabolism: the evidence from human studies. Best Pract Res Clin Endocrinol Metab. 2010 Feb;24(1):117-32. doi: 10.1016/j.beem.2009.08.012.
Houston BL, Hurrie D, Graham J, Perija B, Rimmer E, Rabbani R, Bernstein CN, Turgeon AF, Fergusson DA, Houston DS, Abou-Setta AM, Zarychanski R. Efficacy of iron supplementation on fatigue and physical capacity in non-anaemic iron-deficient adults: a systematic review of randomised controlled trials. BMJ Open. 2018 Apr 5;8(4):e019240. doi: 10.1136/bmjopen-2017-019240.
Hurrell R, Egli I. Iron bioavailability and dietary reference values. Am J Clin Nutr. 2010 May;91(5):1461S-1467S. doi: 10.3945/ajcn.2010.28674F.
Jáuregui-Lobera I. Iron deficiency and cognitive functions. Neuropsychiatr Dis Treat. 2014 Nov 10;10:2087-95. doi: 10.2147/NDT.S72491.
Kapoor MP, Sugita M, Kawaguchi M, Timm D, Kawamura A, Abe A, Okubo T. Influence of iron supplementation on fatigue, mood states and sweating profiles of healthy non-anemic athletes during a training exercise: A double-blind, randomized, placebo-controlled, parallel-group study. Contemp Clin Trials Commun. 2023 Feb 3;32:101084. doi: 10.1016/j.conctc.2023.101084.
Khatiwada S, Gelal B, Baral N, Lamsal M. Association between iron status and thyroid function in Nepalese children. Thyroid Res. 2016 Jan 27;9:2. doi: 10.1186/s13044-016-0031-0.
Leung W, Singh I, McWilliams S, Stockler S, Ipsiroglu OS. Iron deficiency and sleep – A scoping review. Sleep Med Rev. 2020 Jun;51:101274. doi: 10.1016/j.smrv.2020.101274.
Lin CS, Chan LY, Wang JH, Chang CH. Diagnosis and treatment of female alopecia: Focusing on the iron deficiency-related alopecia. Tzu Chi Med J. 2023 Aug 22;35(4):322-328. doi: 10.4103/tcmj.tcmj_95_23.
Liu J, Pu C, Lang L, Qiao L, Abdullahi MA, Jiang C. Molecular pathogenesis of hereditary hemochromatosis. Histol Histopathol. 2016 Aug;31(8):833-40. doi: 10.14670/HH-11-762.
Luo J, Wang X, Yuan L, Guo L. Iron Deficiency, a Risk Factor of Thyroid Disorders in Reproductive-Age and Pregnant Women: A Systematic Review and Meta-Analysis. Front Endocrinol (Lausanne). 2021 Feb 25;12:629831. doi: 10.3389/fendo.2021.629831.
Lynch SR. Interaction of iron with other nutrients. Nutr Rev. 1997 Apr;55(4):102-10. doi: 10.1111/j.1753-4887.1997.tb06461.x.
Macher S, Herster C, Holter M, Moritz M, Matzhold EM, Stojakovic T, Pieber TR, Schlenke P, Drexler C, Amrein K. The Effect of Parenteral or Oral Iron Supplementation on Fatigue, Sleep, Quality of Life and Restless Legs Syndrome in Iron-Deficient Blood Donors: A Secondary Analysis of the IronWoMan RCT. Nutrients. 2020 May 5;12(5):1313. doi: 10.3390/nu12051313.
Meng SH, Zhou HB, Li X, Wang MX, Kang LX, Fu JM, Li X, Li XT, Zhao YS. Association Between Dietary Iron Intake and Serum Ferritin and Severe Headache or Migraine. Front Nutr. 2021 Jul 6;8:685564. doi: 10.3389/fnut.2021.685564.
Miller EM. Iron status and reproduction in US women: National Health and Nutrition Examination Survey, 1999-2006. PLoS One. 2014 Nov 6;9(11):e112216. doi: 10.1371/journal.pone.0112216.
Murat S, Ali U, Serdal K, Süleyman D, İlknur P, Mehmet S, Bahattin A, Tunahan U. Assessment of subjective sleep quality in iron deficiency anaemia. Afr Health Sci. 2015 Jun;15(2):621-7. doi: 10.4314/ahs.v15i2.40.
Neumann SN, Li JJ, Yuan XD, Chen SH, Ma CR, Murray-Kolb LE, Shen Y, Wu SL, Gao X. Anemia and insomnia: a cross-sectional study and meta-analysis. Chin Med J (Engl). 2020 Dec 21;134(6):675-681. doi: 10.1097/CM9.0000000000001306.
Oppenheimer SJ. Iron and its relation to immunity and infectious disease. J Nutr. 2001 Feb;131(2S-2):616S-633S; discussion 633S-635S. doi: 10.1093/jn/131.2.616S.
Pamuk GE, Top MŞ, Uyanık MŞ, Köker H, Akker M, Ak R, Yürekli ÖA, Çelik Y. Is iron-deficiency anemia associated with migraine? Is there a role for anxiety and depression? Wien Klin Wochenschr. 2016 Dec;128(Suppl 8):576-580. doi: 10.1007/s00508-015-0740-8.
Park SY, Na SY, Kim JH, Cho S, Lee JH. Iron plays a certain role in patterned hair loss. J Korean Med Sci. 2013 Jun;28(6):934-8. doi: 10.3346/jkms.2013.28.6.934.
Radtke H, Tegtmeier J, Röcker L, Salama A, Kiesewetter H. Daily doses of 20 mg of elemental iron compensate for iron loss in regular blood donors: a randomized, double-blind, placebo-controlled study. Transfusion. 2004 Oct;44(10):1427-32. doi: 10.1111/j.1537-2995.2004.04074.x.
Recommendations to prevent and control iron deficiency in the United States. Centers for Disease Control and Prevention. MMWR Recomm Rep. 1998 Apr 3;47(RR-3):1-29.
Reddy K V, Shastry S, Raturi M, Baliga B P. Impact of Regular Whole-Blood Donation on Body Iron Stores. Transfus Med Hemother. 2020 Feb;47(1):75-79. doi: 10.1159/000499768.
Rossander-Hultén L, Brune M, Sandström B, Lönnerdal B, Hallberg L. Competitive inhibition of iron absorption by manganese and zinc in humans. Am J Clin Nutr. 1991 Jul;54(1):152-6. doi: 10.1093/ajcn/54.1.152.
Suharno D, West CE, Muhilal, Karyadi D, Hautvast JG. Supplementation with vitamin A and iron for nutritional anaemia in pregnant women in West Java, Indonesia. Lancet. 1993 Nov 27;342(8883):1325-8. doi: 10.1016/0140-6736(93)92246-p.
Swaminathan S, Fonseca VA, Alam MG, Shah SV. The role of iron in diabetes and its complications. Diabetes Care. 2007 Jul;30(7):1926-33. doi: 10.2337/dc06-2625.
Tayyebi A, Poursadeghfard M, Nazeri M, Pousadeghfard T. Is There Any Correlation between Migraine Attacks and Iron Deficiency Anemia? A Case-Control Study. Int J Hematol Oncol Stem Cell Res. 2019 Jul 1;13(3):164-171.
Treister-Goltzman Y, Yarza S, Peleg R. Iron Deficiency and Nonscarring Alopecia in Women: Systematic Review and Meta-Analysis. Skin Appendage Disord. 2022 Mar;8(2):83-92. doi: 10.1159/000519952.
Trotti LM, Bhadriraju S, Becker LA. Iron for restless legs syndrome. Cochrane Database Syst Rev. 2012 May 16;5(5):CD007834. doi: 10.1002/14651858.CD007834.pub2. Update in: Cochrane Database Syst Rev. 2019 Jan 04;1:CD007834.
Vaucher P, Druais PL, Waldvogel S, Favrat B. Effect of iron supplementation on fatigue in nonanemic menstruating women with low ferritin: a randomized controlled trial. CMAJ. 2012 Aug 7;184(11):1247-54. doi: 10.1503/cmaj.110950.
von Haehling S, Jankowska EA, van Veldhuisen DJ, Ponikowski P, Anker SD. Iron deficiency and cardiovascular disease. Nat Rev Cardiol. 2015 Nov;12(11):659-69. doi: 10.1038/nrcardio.2015.109.
Wang M. Iron Deficiency and Other Types of Anemia in Infants and Children. Am Fam Physician. 2016 Feb 15;93(4):270-8.
Winter WE, Bazydlo LA, Harris NS. The molecular biology of human iron metabolism. Lab Med. 2014 Spring;45(2):92-102. doi: 10.1309/lmf28s2gimxnwhmm.
Yang W, Li B, Dong X, Zhang XQ, Zeng Y, Zhou JL, Tang YH, Xu JJ. Is heme iron intake associated with risk of coronary heart disease? A meta-analysis of prospective studies. Eur J Nutr. 2014;53(2):395-400. doi: 10.1007/s00394-013-0535-5.
Zečkanović A, Kavčič M, Prelog T, Šmid A, Jazbec J. Micronized, Microencapsulated Ferric Iron Supplementation in the Form of >Your< Iron Syrup Improves Hemoglobin and Ferritin Levels in Iron-Deficient Children: Double-Blind, Randomized Clinical Study of Efficacy and Safety. Nutrients. 2021 Mar 26;13(4):1087. doi: 10.3390/nu13041087.
Zhang C. Essential functions of iron-requiring proteins in DNA replication, repair and cell cycle control. Protein Cell. 2014 Oct;5(10):750-60. doi: 10.1007/s13238-014-0083-7.