Table of Contents[Hide][Show]
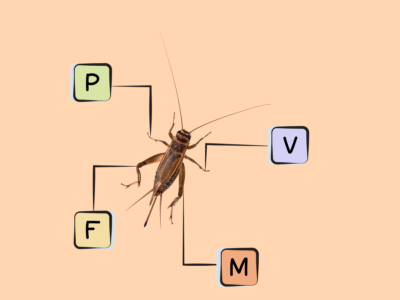
Top 5 Common Food Sources of Phosphorus
Looking to get extra phosphorus in your diet? Look no further! My team and I have crunched the numbers and did all the math to determine the top 5 common food sources of this mineral, per serving. Even though phosphorus is present in most foods, there’s very few foods that provide half of the daily value of phosphorus per serving, so it’s important to choose a variety of phosphorus rich foods that deliver smaller amounts, and and sprinkle those throughout the day. Getting enough phosphorus as part of a healthy balanced diet is important since a large collection of studies show that getting nutrients from dietary supplements or multivitamins doesn’t improve health outcomes compared to getting nutrients from foods!
| Rank | Food | Nutrivore Score | Serving Size (Raw) | Phosphorus (mg/serving) | % Daily Value |
|---|---|---|---|---|---|
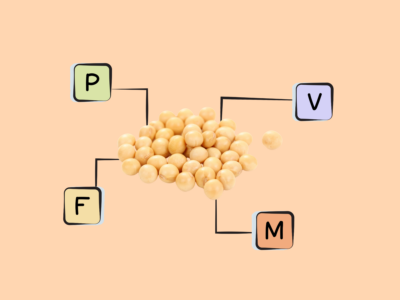
| 1 | Soybeans, Mature Seeds | 326 | 1/2 cup | 654.7 | 52 |
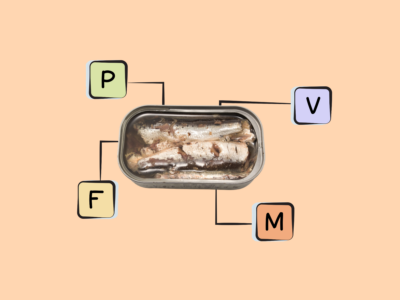
| 2 | Atlantic Sardines, Canned in Oil, w/ bone | 654 | 4 oz / 115 g | 563.5 | 45 |
| 3 | Hemp Seeds, Hulled | 415 | 1 oz / 28 g | 467.8 | 37 |
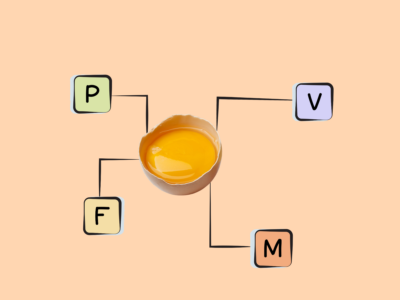
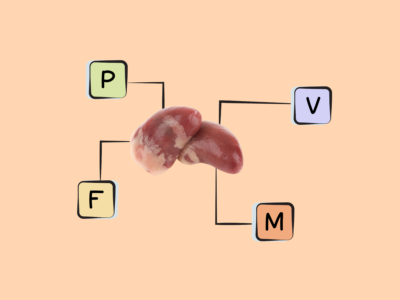
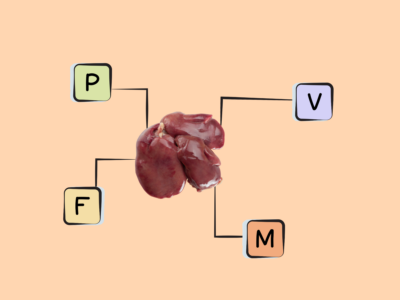
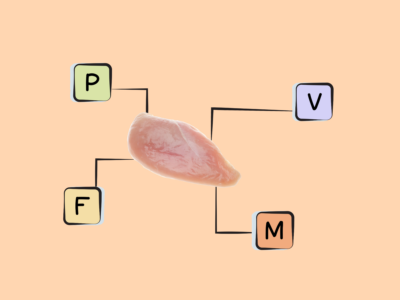
| 4 | Chicken Egg, Yolk | 342 | 100 g (6 eggs) | 390.0 | 31 |
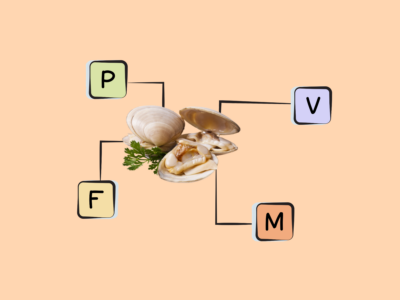
| 5 | Scallops, Mixed Species | 645 | 4 oz / 115 g | 384.1 | 31 |
Want to know more about this essential mineral including what phosphorus does in the body, how much phosphorus we need, what happens if we have low phosphorus levels or if we get too much, and even more high-phosphorus foods? Keep reading to learn all there is to know!
Learn What Foods Are the Best Sources of Every Nutrient

The Top 25 Foods for Every Nutrient
The Top 25 Foods for Every Nutrient e-book is a well-organized, easy-to-use, grocery store-friendly guide to help you choose foods that fit your needs of 43 important nutrients while creating a balanced nutrient-dense diet.
Get two “Top 25” food lists for each nutrient, plus you’ll find RDA charts for everyone, informative visuals, fun facts, serving sizes and the 58 foods that are Nutrient Super Stars!
Buy now for instant digital access.
What Is Phosphorus and What Does It Do?
Phosphorus is a highly abundant mineral in the human body, playing important structural roles as a component of bones (as calcium phosphate crystals), nucleic acids (as sugar-phosphate backbones), and cell membranes (as the phospholipid bilayer). It also helps maintain the body’s acid-base balance, and is needed to create a molecule involved in oxygen delivery to tissues. A number of enzymes, hormones, and cell-signaling molecules also rely on phosphorus (via the process of phosphorylation) to become activated and carry out their functions.
Most research on the health effects of phosphorus have pointed to problems with excess intake. Studies suggest that excess dietary phosphorus is associated with increased risk of all-cause mortality, cardiovascular disease, and osteoporosis—possibly due to the effects phosphorus has on the regulation of certain hormones (including vitamin D and parathyroid hormone) and cell differentiation. When it comes to bone health, getting enough calcium appears particularly important for protecting against the effects of high phosphorus consumption!
Learn more about phosphorus here.
Phosphorus Deficiency
A 2011 study evaluated American’s usual nutrient intake including nutrients that are naturally-occurring in foods, from fortified and enriched foods, and from supplements. The results indicated that 2.0% of American adults usual diet falls short of the Estimated Average Requirement (EAR) for phosphorus intake.
Groups At Risk
Due to its abundance in foods (as well as its high bioavailability), phosphorus deficiency is rare. Even when dietary intake is low, the body is generally able to compensate by increasing renal absorption so that blood levels of phosphorus can remain stable.
However, those at higher risk of phosphorus deficiency include:
- individuals with inherited renal phosphorus-wasting disorders,
- alcoholics,
- people with respiratory alkalosis,
- anorexic patients on high-calorie re-feeding regimens, and
- diabetics recovering from diabetic ketoacidosis.
Learn more here.
Symptoms of Deficiency
Low blood phosphorus, known as hypophosphatemia, can lead to symptoms such as muscle weakness, numbness in the extremities, bone pain and fragility, loss of appetite, and respiratory failure. It also increases susceptibility to infections and causes bone softening. In severe, untreated cases, hypophosphatemia can become life-threatening.
Learn more here.
Problems From Too Much Phosphorus
High phosphorus intake and elevated blood levels (hyperphosphatemia) have been linked to adverse health outcomes, including increased all-cause mortality, cardiovascular disease, osteoporosis, and kidney disease to name a few. Even levels at the high end of normal are associated with greater risks of cardiovascular disease, atrial fibrillation, heart failure, and left ventricular hypertrophy. Impaired kidney function is a common cause of hyperphosphatemia, as the kidneys play a vital role in excreting excess phosphorus (in this case dialysis can help remove the excess). Problems caused by excess phosphorus likely stem from the ways phosphorus is regulated—particularly the secretion or action of parathyroid hormone, vitamin D, and fibroblast growth factor 23. High phosphorus levels can cause disordered regulation of these hormones, such as impairing the synthesis of active vitamin D (in turn increasing the risk of kidney disease, heart disease, and calcium phosphate buildup in the organs and other soft tissue). It can also lead to vascular calcification, bone mineral loss, and other complications. Interestingly, the calcium-to-phosphorus dietary ratio may be more important than phosphorus intake alone when it comes to influencing skeletal health, with sufficient calcium potentially mitigating phosphorus’s negative effects. To limit risks, the tolerable upper intake level for phosphorus is set at 4,000 mg daily for adults under 70 and 3,000 mg for older adults.
Learn more here.
How Much Phosphorus Do We Need?
The following table summarizes the current recommended amounts of phosphorus, based on age, gender, or situation. Keep in mind that the Food and Drug Administration (FDA) does not require food labels to list phosphorus content unless phosphorus has been added to the food.
| 0 – 6 months | |||||
| 6 months to < 12 months | |||||
| 1 yr – 3 yrs | |||||
| 4 yrs – 8 yrs | |||||
| 9 yrs – 13 yrs | |||||
| 14 yrs – 18 yrs | |||||
| 19 yrs – 50 yrs | |||||
| 51+ yrs | |||||
| Pregnant (14 – 18 yrs) | |||||
| Pregnant (19 – 30 yrs) | |||||
| Pregnant (31 – 50 yrs) | |||||
| Lactating (14 – 18 yrs) | |||||
| Lactating (19 – 30 yrs) | |||||
| Lactating (31 – 50 yrs) |
Nutrient Daily Values
Nutrition requirements and recommended nutrient intake for infants, children, adolescents, adults, mature adults, and pregnant and lactating individuals.
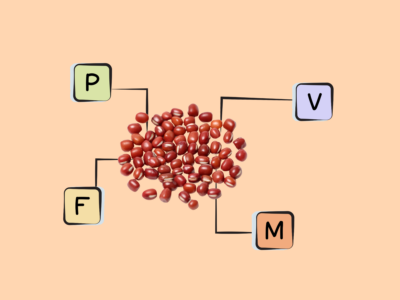
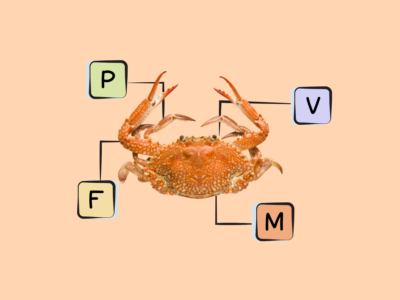
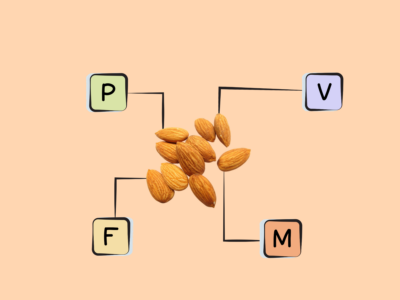
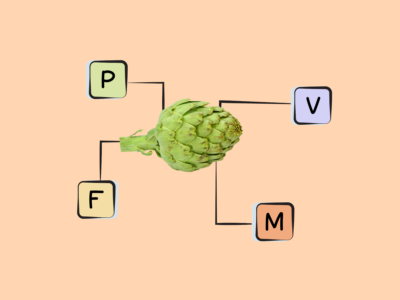
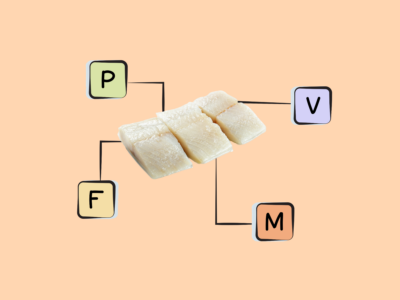
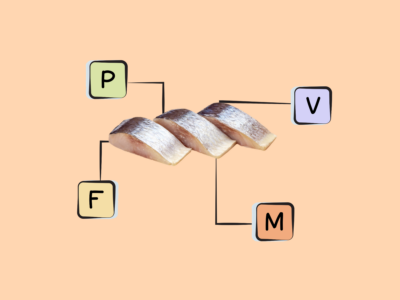
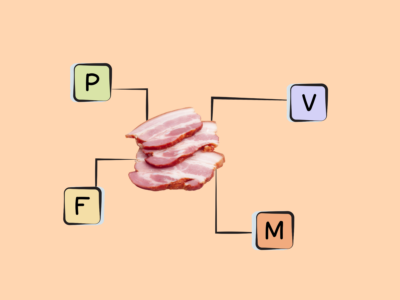
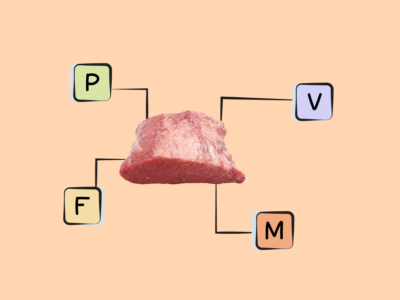
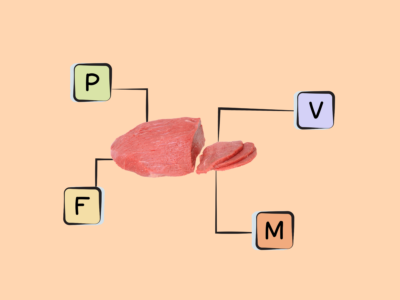
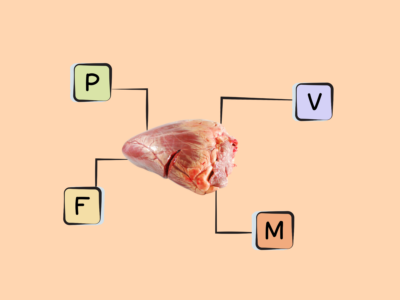
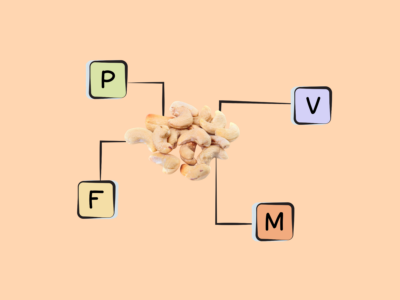
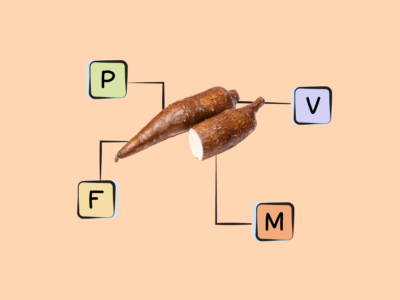
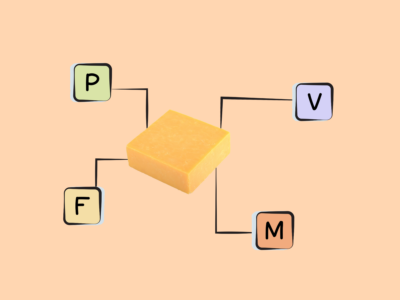
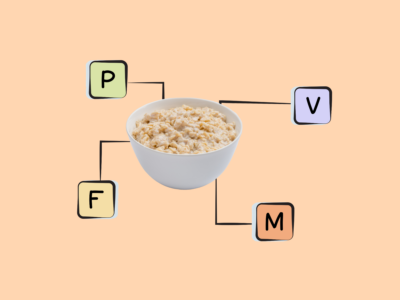
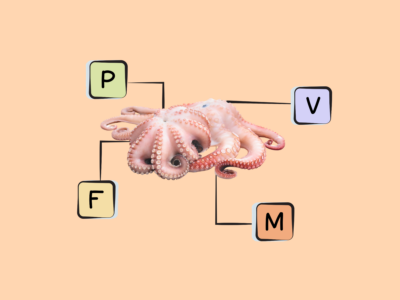
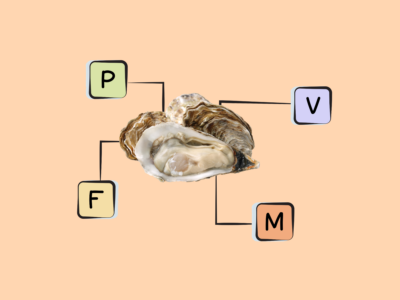
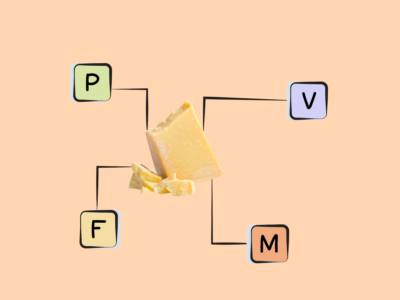
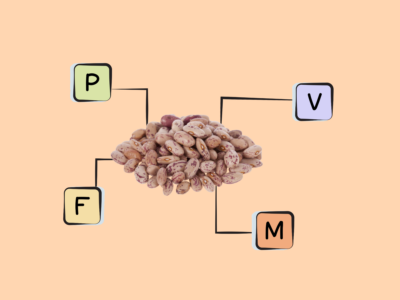
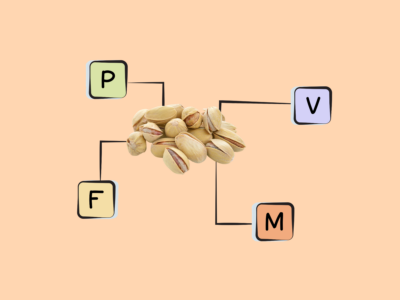
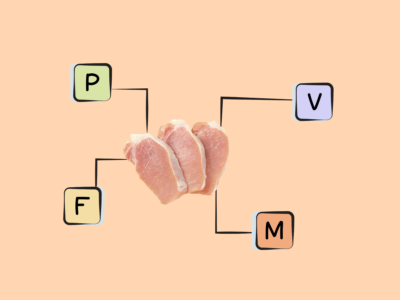
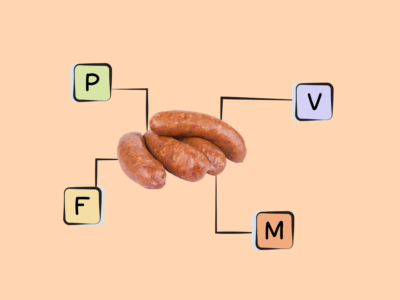
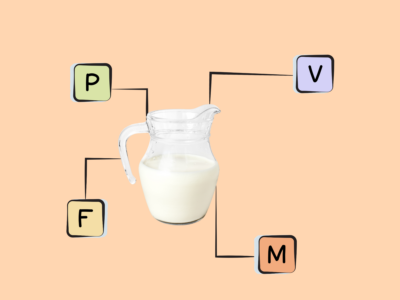
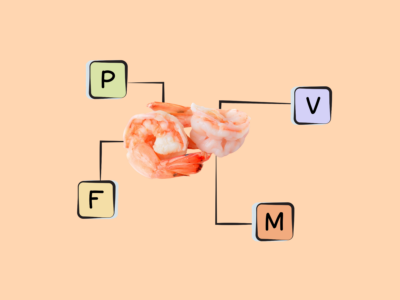
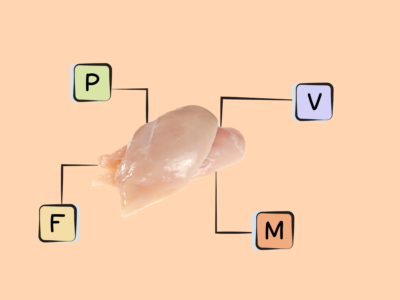
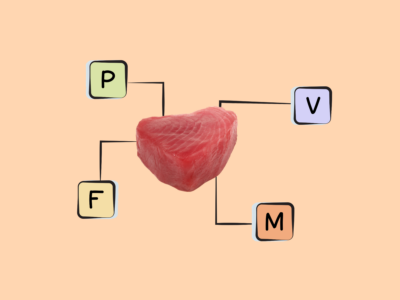
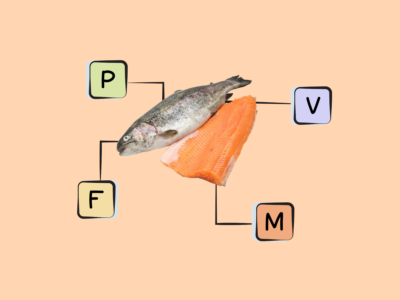
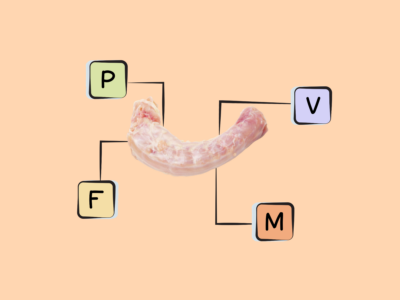
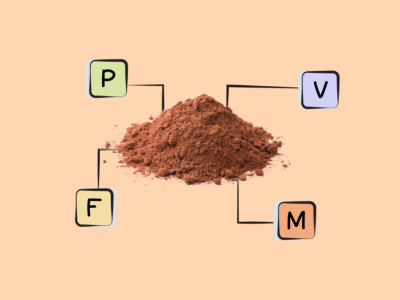
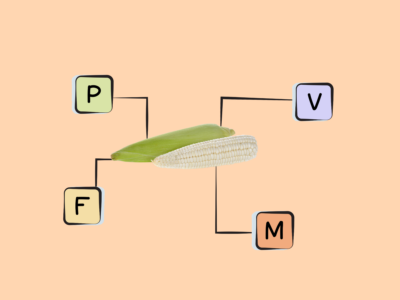
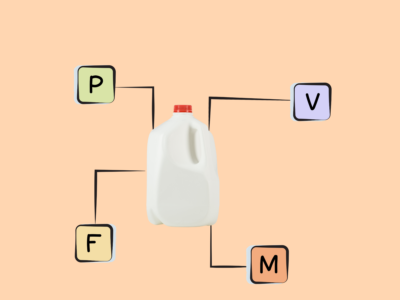
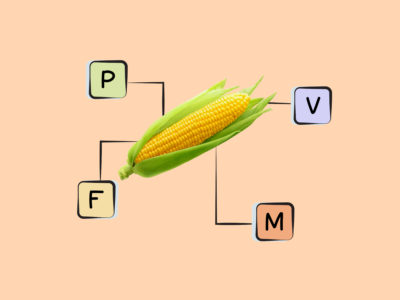
More Food Sources of Phosphorus
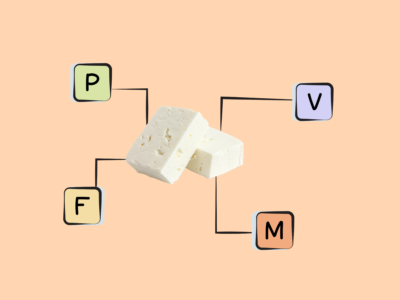
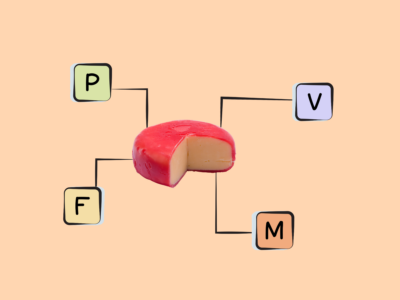
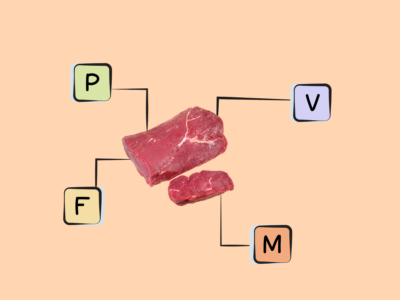
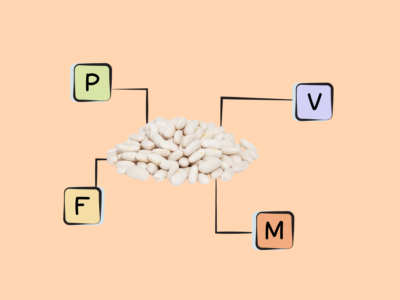
Phosphorous is present in most foods, but it’s particularly abundant in protein-rich items such as dairy products, fish, shellfish, poultry, organ meats, seeds, and legumes. Whole grains and bakery products such as breads and tortillas are also common food sources of phosphorus. This mineral is also found in many common food additives (such as the phosphate additive phosphoric acid used in soft drinks), so it’s often abundant in fast foods and processed foods (anything from cereals to waffles to ice cream).
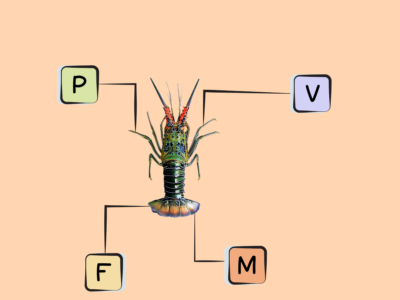
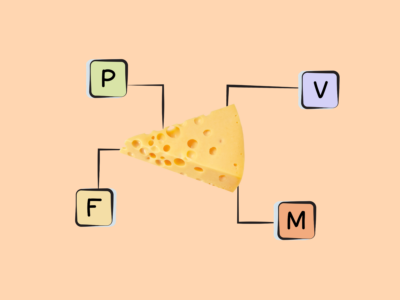
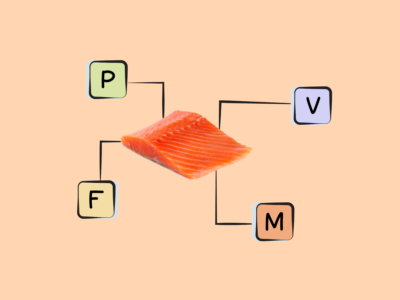
Best Food Sources of Phosphorus
The following foods have high concentrations of phosphorus, containing at least 50% of the recommended dietary allowance per serving, making them our best food sources of this valuable mineral!
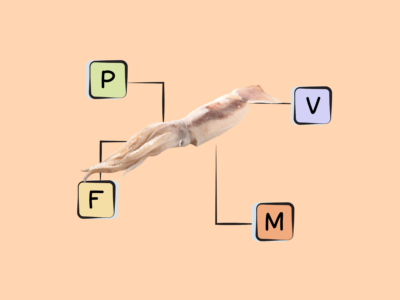
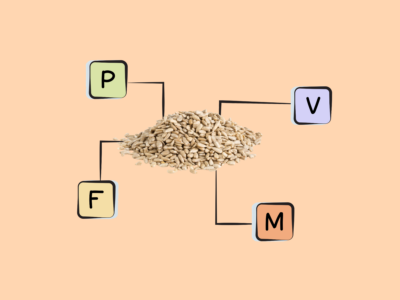
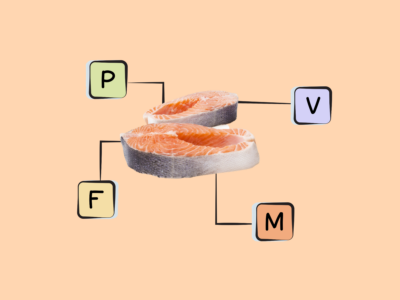
Good Food Sources of Phosphorus
The following foods are excellent or good sources of phosphorus, containing at least 10% (and up to 50%) of the daily value per serving. Just missing the list at 9% is lentils!
Top 5 Common Food Sources
If you’re looking for top 5 common food sources of other important nutrients check out these posts!
cITATIONS
Expand to see all scientific references for this article.
Alizadeh Naderi AS, Reilly RF. Hereditary disorders of renal phosphate wasting. Nat Rev Nephrol. 2010 Nov;6(11):657-65. doi: 10.1038/nrneph.2010.121.
Amanzadeh J, Reilly RF Jr. Hypophosphatemia: an evidence-based approach to its clinical consequences and management. Nat Clin Pract Nephrol. 2006 Mar;2(3):136-48. doi: 10.1038/ncpneph0124.
Bansal N, Katz R, de Boer IH, Kestenbaum B, Siscovick DS, Hoofnagle AN, Tracy R, Laughlin GA, Criqui MH, Budoff MJ, Li D, Ix JH. Influence of estrogen therapy on calcium, phosphorus, and other regulatory hormones in postmenopausal women: the MESA study. J Clin Endocrinol Metab. 2013 Dec;98(12):4890-8. doi: 10.1210/jc.2013-2286.
Calvo MS, Park YK. Changing phosphorus content of the U.S. diet: potential for adverse effects on bone. J Nutr. 1996 Apr;126(4 Suppl):1168S-80S. doi: 10.1093/jn/126.suppl_4.1168S
Calvo MS, Tucker KL. Is phosphorus intake that exceeds dietary requirements a risk factor in bone health? Ann N Y Acad Sci. 2013 Oct;1301:29-35. doi: 10.1111/nyas.12300.
Calvo MS, Uribarri J. Public health impact of dietary phosphorus excess on bone and cardiovascular health in the general population. Am J Clin Nutr. 2013 Jul;98(1):6-15. doi: 10.3945/ajcn.112.053934.
Chang AR, Lazo M, Appel LJ, Gutiérrez OM, Grams ME. High dietary phosphorus intake is associated with all-cause mortality: results from NHANES III. Am J Clin Nutr. 2014 Feb;99(2):320-7. doi: 10.3945/ajcn.113.073148. Epub 2013 Nov 13.
Da J, Xie X, Wolf M, Disthabanchong S, Wang J, Zha Y, Lv J, Zhang L, Wang H. Serum Phosphorus and Progression of CKD and Mortality: A Meta-analysis of Cohort Studies. Am J Kidney Dis. 2015 Aug;66(2):258-65. doi: 10.1053/j.ajkd.2015.01.009.
de Boer IH, Rue TC, Kestenbaum B. Serum phosphorus concentrations in the third National Health and Nutrition Examination Survey (NHANES III). Am J Kidney Dis. 2009 Mar;53(3):399-407. doi: 10.1053/j.ajkd.2008.07.036.
Dhingra R, Sullivan LM, Fox CS, Wang TJ, D’Agostino RB Sr, Gaziano JM, Vasan RS. Relations of serum phosphorus and calcium levels to the incidence of cardiovascular disease in the community. Arch Intern Med. 2007 May 14;167(9):879-85. doi: 10.1001/archinte.167.9.879.
Foley RN, Collins AJ, Herzog CA, Ishani A, Kalra PA. Serum phosphate and left ventricular hypertrophy in young adults: the coronary artery risk development in young adults study. Kidney Blood Press Res. 2009;32(1):37-44. doi: 10.1159/000203348.
Fulgoni VL 3rd, Keast DR, Bailey RL, Dwyer J. Foods, fortificants, and supplements: Where do Americans get their nutrients? J Nutr. 2011 Oct;141(10):1847-54. doi: 10.3945/jn.111.142257. Epub 2011 Aug 24. PMID: 21865568; PMCID: PMC3174857.
Grimm M, Müller A, Hein G, Fünfstück R, Jahreis G. High phosphorus intake only slightly affects serum minerals, urinary pyridinium crosslinks and renal function in young women. Eur J Clin Nutr. 2001 Mar;55(3):153-61. doi: 10.1038/sj.ejcn.1601131.
Heaney RP, Nordin BE. Calcium effects on phosphorus absorption: implications for the prevention and co-therapy of osteoporosis. J Am Coll Nutr. 2002 Jun;21(3):239-44. doi: 10.1080/07315724.2002.10719216.
Institute of Medicine (US) Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. Washington (DC): National Academies Press (US); 1997.
Ito S, Ishida H, Uenishi K, Murakami K, Sasaki S. The relationship between habitual dietary phosphorus and calcium intake, and bone mineral density in young Japanese women: a cross-sectional study. Asia Pac J Clin Nutr. 2011;20(3):411-7.
Jono S, McKee MD, Murry CE, Shioi A, Nishizawa Y, Mori K, Morii H, Giachelli CM. Phosphate regulation of vascular smooth muscle cell calcification. Circ Res. 2000 Sep 29;87(7):E10-7. doi: 10.1161/01.res.87.7.e10.
Kemi VE, Kärkkäinen MU, Rita HJ, Laaksonen MM, Outila TA, Lamberg-Allardt CJ. Low calcium:phosphorus ratio in habitual diets affects serum parathyroid hormone concentration and calcium metabolism in healthy women with adequate calcium intake. Br J Nutr. 2010 Feb;103(4):561-8. doi: 10.1017/S0007114509992121.
Lopez FL, Agarwal SK, Grams ME, Loehr LR, Soliman EZ, Lutsey PL, Chen LY, Huxley RR, Alonso A. Relation of serum phosphorus levels to the incidence of atrial fibrillation (from the Atherosclerosis Risk In Communities [ARIC] study). Am J Cardiol. 2013 Mar 15;111(6):857-62. doi: 10.1016/j.amjcard.2012.11.045.
Martin A, David V, Quarles LD. Regulation and function of the FGF23/klotho endocrine pathways. Physiol Rev. 2012 Jan;92(1):131-55. doi: 10.1152/physrev.00002.2011.
Menon MC, Ix JH. Dietary phosphorus, serum phosphorus, and cardiovascular disease. Ann N Y Acad Sci. 2013 Oct;1301:21-6. doi: 10.1111/nyas.12283.
O’Seaghdha CM, Hwang SJ, Muntner P, Melamed ML, Fox CS. Serum phosphorus predicts incident chronic kidney disease and end-stage renal disease. Nephrol Dial Transplant. 2011 Sep;26(9):2885-90. doi: 10.1093/ndt/gfq808.
Paunier L. Effect of magnesium on phosphorus and calcium metabolism. Monatsschr Kinderheilkd. 1992 Sep;140(9 Suppl 1):S17-20.
Phosphorus: Fact Sheet for Health Professionals. National Institutes of Health (NIH) Office of Dietary Supplements. 26 Mar 2021.
Pinheiro MM, Schuch NJ, Genaro PS, Ciconelli RM, Ferraz MB, Martini LA. Nutrient intakes related to osteoporotic fractures in men and women–the Brazilian Osteoporosis Study (BRAZOS). Nutr J. 2009 Jan 29;8:6. doi: 10.1186/1475-2891-8-6.
Rennenberg RJ, Kessels AG, Schurgers LJ, van Engelshoven JM, de Leeuw PW, Kroon AA. Vascular calcifications as a marker of increased cardiovascular risk: a meta-analysis. Vasc Health Risk Manag. 2009;5(1):185-97. doi: 10.2147/vhrm.s4822.
Shuto E, Taketani Y, Tanaka R, Harada N, Isshiki M, Sato M, Nashiki K, Amo K, Yamamoto H, Higashi Y, Nakaya Y, Takeda E. Dietary phosphorus acutely impairs endothelial function. J Am Soc Nephrol. 2009 Jul;20(7):1504-12. doi: 10.1681/ASN.2008101106.
Takeda E, Yamamoto H, Yamanaka-Okumura H, Taketani Y. Dietary phosphorus in bone health and quality of life. Nutr Rev. 2012 Jun;70(6):311-21. doi: 10.1111/j.1753-4887.2012.00473.x.
Tonelli M, Sacks F, Pfeffer M, Gao Z, Curhan G; Cholesterol And Recurrent Events Trial Investigators. Relation between serum phosphate level and cardiovascular event rate in people with coronary disease. Circulation. 2005 Oct 25;112(17):2627-33. doi: 10.1161/CIRCULATIONAHA.105.553198.
Tuttle KR, Short RA. Longitudinal relationships among coronary artery calcification, serum phosphorus, and kidney function. Clin J Am Soc Nephrol. 2009 Dec;4(12):1968-73. doi: 10.2215/CJN.01250209.
Umeukeje EM, Merighi JR, Browne T, Wild M, Alsmaan H, Umanath K, Lewis JB, Wallston KA, Cavanaugh KL. Health care providers’ support of patients’ autonomy, phosphate medication adherence, race and gender in end stage renal disease. J Behav Med. 2016 Dec;39(6):1104-1114. doi: 10.1007/s10865-016-9745-7. Epub 2016 May 11.
Uribarri J, Calvo MS. Dietary phosphorus excess: a risk factor in chronic bone, kidney, and cardiovascular disease? Adv Nutr. 2013 Sep 1;4(5):542-4. doi: 10.3945/an.113.004234.
Zhang D, Maalouf NM, Adams-Huet B, Moe OW, Sakhaee K. Effects of sex and postmenopausal estrogen use on serum phosphorus levels: a cross-sectional study of the National Health and Nutrition Examination Survey (NHANES) 2003-2006. Am J Kidney Dis. 2014 Feb;63(2):198-205. doi: 10.1053/j.ajkd.2013.07.012.