Key Takeaways (expand)
- Thiamin (sometimes spelled thiamine, and also called vitamin B1) is an essential vitamin and the first water-soluble vitamin ever identified.
- In the form of thiamin pyrophosphate, thiamin serves as a cofactor for four enzyme complexes involved metabolizing carbohydrates and branched-chain amino acids.
- Because thiamin is needed for synthesizing ribose from glucose, it’s necessary for the production of RNA and DNA.
- Like other B vitamins, thiamin plays an important role in the Krebs cycle—specifically, in converting pyruvate into acetyl CoA, the energy source for the Krebs cycle itself.
- Thiamin is also needed for maintaining normal muscle function, including that of the heart.
- Among people with glucose intolerance or type 2 diabetes, high-dose thiamin supplements have been shown to prevent increases in fasting blood sugar and insulin, as well as potentially protect against renal complications.
- Higher thiamin intake is associated with lower risk of cataracts.
- Low levels of thiamin (and subsequently thiamin-dependent enzymes) are associated with a higher risk of Alzheimer’s disease, although more controlled research is needed in humans to test whether increasing thiamin intake could improve cognitive impairments.
- Some evidence suggests thiamin therapy can help treat sepsis, including reducing mortality risk, improving lactate clearance, and protecting against progressive organ dysfunction in septic patients.
- Fast-growing tumors have high thiamin demands and can consequently induce thiamin deficiency in cancer patients, leading to some recommendations to supplement with this nutrient; however, it’s also possible that supplementing with thiamin could further fuel the growth of those tumors. More research is needed to understand the relationship between thiamin and cancer.
- Severe thiamin deficiency causes beriberi, a disease that can affect the cardiovascular system and/or nervous system.
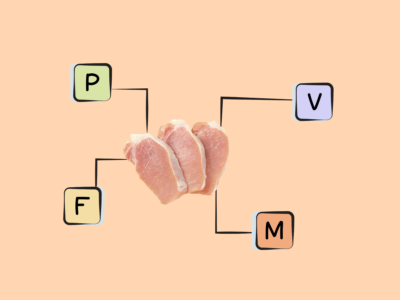
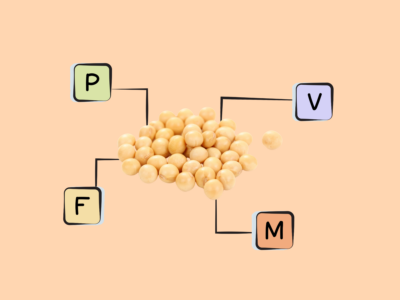
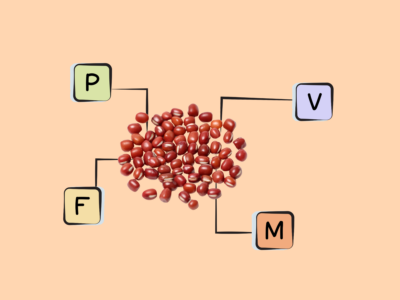
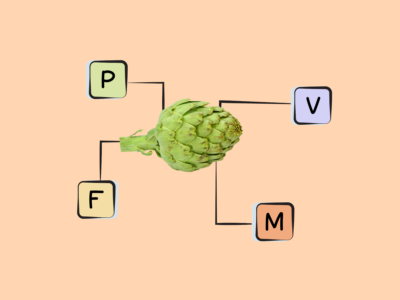
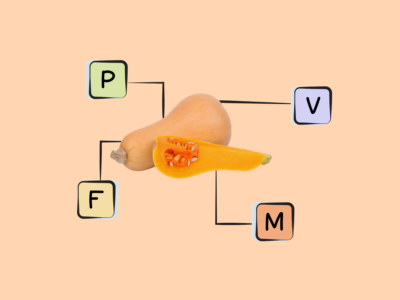
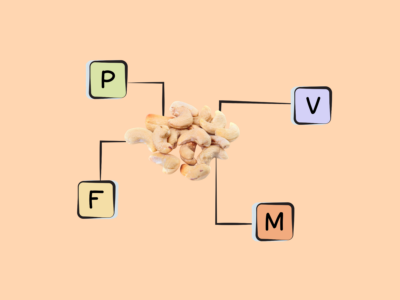
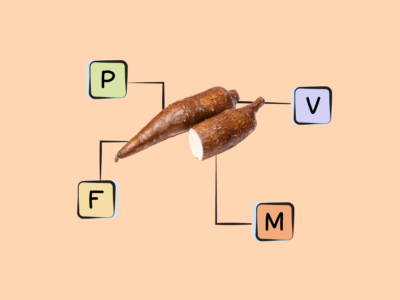
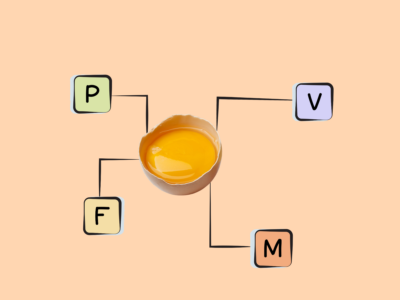
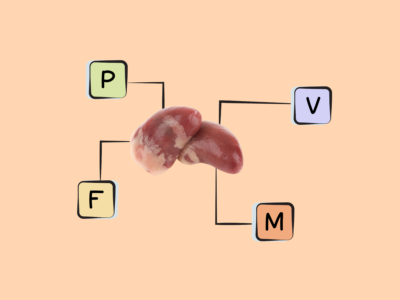
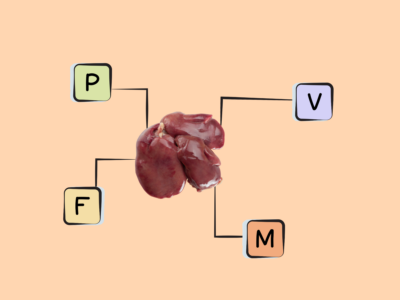
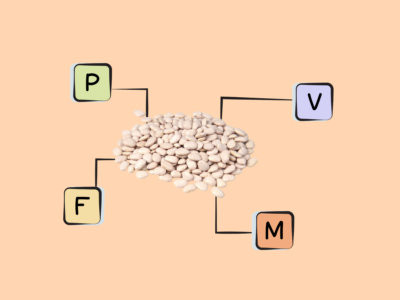
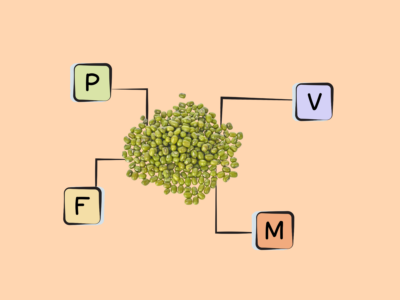
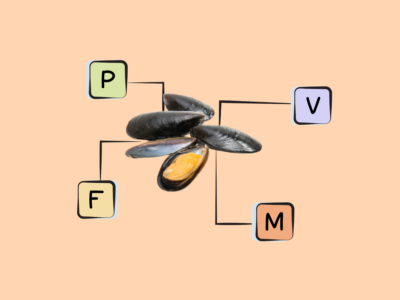
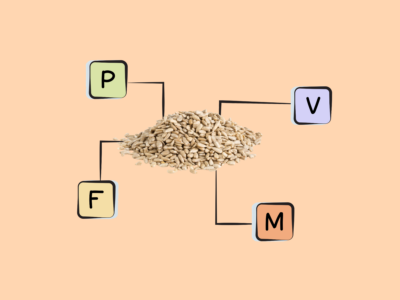
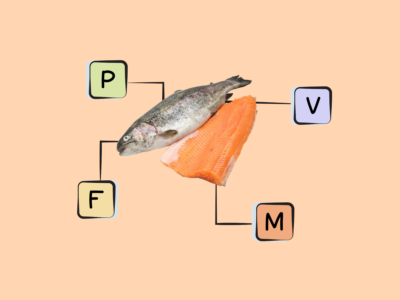
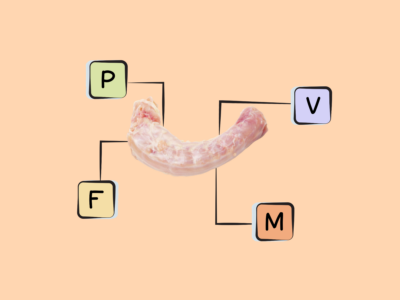
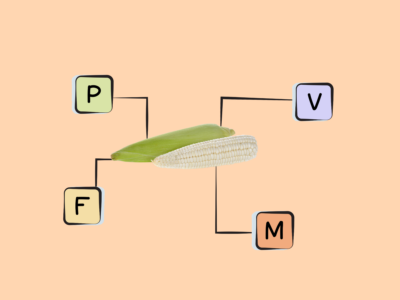
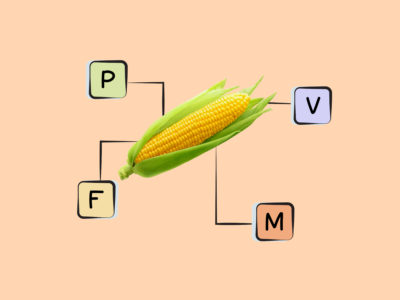
- Good sources of thiamin include organ meats, pork, squash, seeds, fish, yeast, legumes, and whole grains.
Table of Contents[Hide][Show]
- What are The Biological Roles of Vitamin B1 (Thiamin)?
- What are the Health Effects of Vitamin B1 (Thiamin) Deficiency?
- What are the Problems From Too Much Vitamin B1 (Thiamin)?
- How Much Vitamin B1 (Thiamin) Do We Need?
- What are the Best Food Sources of Vitamin B1 (Thiamin)?
- What are the Good Food Sources of Vitamin B1 (Thiamin)
Thiamin (sometimes spelled thiamine, and also called vitamin B1) is one of eight B vitamins, and was the first water-soluble vitamin ever identified.
Interestingly, severe thiamin deficiency—called beriberi—was initially believed to be an infectious disease, and was the subject of failed experiments attempting to transmit the disease by injecting animals with bacteria cultured from beriberi-inflicted humans. A Japanese physician first challenged this microbial theory in 1884, when he discovered that changing the diets of sailors on naval ships (from white rice only, to a more diverse diet of barley, bread, meat, and vegetables) eliminated the beriberi that was previously plaguing sailors on long voyages. But, he mistakenly concluded the issue was protein intake, and was unable identify the real cure for beriberi. Thiamin was more precisely linked to nutrition in the late 1800s, when a Dutch scientist named Christiaan Eijkman noticed that the chickens in his laboratory developed beriberi-like symptoms when fed white polished rice, but remained healthy when fed either brown unpolished rice or the rice polishings that had been discarded from white rice. This led to further investigations that determined an essential nutrient existed in the outer layers of rice grain (and, later, in many other foods!). Thiamin was initially named “aneurin,” short for “anti-neuritic vitamin” (referring to its ability to prevent the nervous system dysfunction seen with beriberi), and was later renamed thiamin from a combination of the words thio (referring to sulfur) and amine (referring to the amino group in its chemical structure).
Like other B vitamins, it plays an important role in energy metabolism—breaking down the carbohydrates, fat, and protein we eat for use as fuel (hence why B-complex vitamins are often nicknamed the “energy vitamins!”), as well as neurotransmitter production, cellular function, and a wide variety of organ functions.
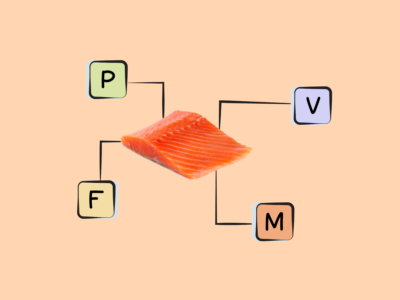
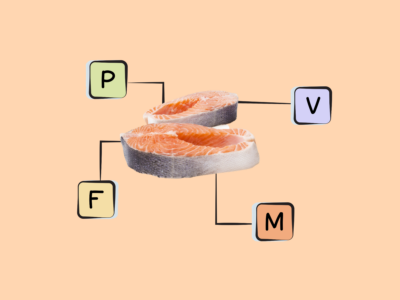
Rich sources include organ meat, pork, seeds, squash, yeasts, fish (especially trout, mackerel, salmon, and tuna), legumes, and whole grains (although processing grains significantly reduces their thiamin content). Some foods are also fortified with thiamin, such as breakfast cereals and breads.
Want to know the top 25 foods for this awesome nutrient?

The Top 25 Foods for Every Nutrient
The Top 25 Foods for Every Nutrient e-book is a well-organized, easy-to-use, grocery store-friendly guide to help you choose foods that fit your needs of 43 important nutrients while creating a balanced nutrient-dense diet.
Get two “Top 25” food lists for each nutrient, plus you’ll find RDA charts for everyone, informative visuals, fun facts, serving sizes and the 58 foods that are Nutrient Super Stars!
Buy now for instant digital access.
What are The Biological Roles of Vitamin B1 (Thiamin)?
Thiamin serves as an important cofactor for a number of metabolic processes—especially in the active form thiamin pyrophosphate, which is synthesized from free thiamin with the help of magnesium, adenosine triphosphate (ATP), and the enzyme thiamin pyrophosphokinase. As thiamin pyrophosphate, it assists in the metabolism of carbohydrates and branched-chain amino acids (leucine, isoleucine, and valine) by helping four enzyme complexes to do their job: pyruvate dehydrogenase (which converts pyruvate to acetyl-CoA), α-ketoglutarate dehydrogenase (which converts alpha-ketogluterate to succinyl-CoA), branched-chain α-ketoacid dehydrogenase (which converts branched-chain alpha-keto acids to acyl-CoA), and transketolase (which connects the pentose phosphate pathway to glycolysis, by acting on specific phosphate sugars and transferring their transformed versions to aldose receptors). Via its role as a coenzyme, thiamin is also needed for synthesizing ribose from glucose, making it necessary for making RNA and DNA.
Like other B vitamins, it also plays an important role in energy metabolism—particularly the second stage of cellular respiration, called the Krebs cycle or citric acid cycle. The Krebs cycle is an incredibly important series of chemical reactions that all aerobic organisms use to generate energy, through an eight-step process taking place in a cell’s mitochondria. During this cycle, acetate (in the form of acetyl CoA) derived from carbohydrates, fat, or protein undergoes a series of redox, dehydration, hydration, and decarboxylation reactions to produce adenosine triphosphate (ATP), the energy currency for all cells—as well as the waste product carbon dioxide, and reduced forms of NADH and FADH2 (which can then be converted into yet more ATP in the last step of the Krebs cycle: oxidative phosphorylation in the electron transport chain). This is complex biochemistry, but the important part here is that there are a whole lot of chemical reactions required to produce energy for our cells, and B vitamins are essential for that process!
Thiamin’s specific role in the Krebs cycle is in producing acetyl CoA—the energy source for the cycle itself. In the form of thiamin pyrophosphate, thiamin helps convert pyruvate (the end product of glucose metabolism) to acetyl-CoA.
In addition, thiamin is needed for maintaining normal muscle function, including the function of the heart.

Checklists and Planning Tools
Make Nutrivore simple and easy with these handy-dandy planning tools and checklists.
How Does Vitamin B1 (Thiamin) in Health and Disease?
Research suggests that vitamin B1 (thiamin) could help prevent blood sugar and insulin increases in people with disordered glucose metabolism, reduce the risk of cataracts, and improve health and mortality outcomes in patients with sepsis. Because aggressive tumors have high thiamin demands, it’s uncertain whether supplementing with thiamin while having cancer is beneficial due to preventing deficiency, or harmful due to providing more fuel for tumor growth. Insufficient thiamin may increase the risk of Alzheimer’s disease, and when chronic, leads to a deficiency disease called beriberi.
Thiamin and Alzheimer’s Disease
Low levels of thiamin (as well as decreased activity of thiamin-dependent enzymes) is associated with a greater risk of Alzheimer’s disease, and animal studies have shown that thiamin supplementation can significantly improve cognitive impairments. But, clinical studies on humans are limited and have yielded inconsistent results, so more research is needed to confirm whether increasing thiamin intake could have the same beneficial effects for Alzheimer’s disease.
Thiamin and Eye Health
In multiple observational studies, people with the highest thiamin intake had the lowest incidence of cataracts (although cause-and-effect hasn’t been determined).
Thiamin and Type 2 Diabetes
In people who were either glucose intolerant or recently diagnosed with type 2 diabetes, a 2013 study showed that high-dose thiamin supplementation (300 mg daily for six weeks) was able to prevent further increases in fasting blood sugar and insulin levels. Thiamin may have additional benefits for diabetics as well, including preventing the development of renal complications and reducing the excretion of urinary albumin.
Thiamin and Sepsis
Thiamin deficiency is common in patients with sepsis, and thiamin therapy has shown some promise for helping treat this illness (both as an isolated therapy and also in conjunction with other agents).
In observational studies, use of intravenous thiamin is associated with reduced mortality and improved lactate clearance in septic patients, and in randomized controlled trials, parenteral thiamin resulted in lower creatinine concentrations and a lower risk of needing renal replacement therapy. Additional research shows that when intravenous thiamin is combined with intravenous vitamin C and corticosteroids, it can significantly reduce the occurrence of progressive organ dysfunction and mortality in patience with severe sepsis or septic shock.
Thiamin and Cancer
Thiamin has an important, complex relationship with cancer.
Some limited evidence suggests an inverse relationship between thiamin intake and risk of kidney cancer, AKA renal cell carcinoma. A 2018 case-control study including 1142 kidney cancer patients and 1154 matched controls found that higher thiamine intake was associated with lower risk of kidney cancer. However, more research is needed to determine whether this relationship is causal!
In patients with fast-growing tumors, thiamin deficiency becomes more likely due to the high thiamin demands of rapidly dividing cancer cells, as well as the reliance of some cancers on thiamin-dependent enzymes for ribose and nucleic acid synthesis. So, thiamin supplementation is sometimes recommended for cancer patients in order to prevent deficiency. But, consuming high levels of thiamin could theoretically help fuel the growth of malignant tumors by providing them with more ribose phosphate for nucleic acid synthesis (via the thiamin-dependent transkelotase pathway), leading to tumor cell proliferation and potentially reducing the effectiveness of cancer therapies targeted at reducing cancer cell proliferation. Currently, there isn’t enough evidence one way or another to determine the true risk here.
So, until more research is done, high-dose thiamin supplementation might be safest if reserved for cancer patients who are already demonstrating thiamin deficiency, rather than done preventatively.
Thiamin and Obesity
Some research also suggests a role of thiamin in obesity, although the link isn’t fully clear. For example, a 2018 systematic review found that 16 to 47% of obese patients seeking bariatric surgery are thiamin deficient, and that thiamin (in conjunction with magnesium) play a critical role in glucose metabolism and the progression of obesity. More research is needed here!
Thiamin and Genetic Disorders
Thiamin is also useful for managing several genetic diseases that impact carbohydrate and branched-chain amino acid metabolism, including:
- thiamin-responsive pyruvate dehydrogenase complex deficiency (which prevents efficient carbohydrate oxidation, and can lead to lactic acidosis and neurological degeneration),
- maple syrup urine disease (which alters the branch-chain amino acid catabolic pathway and leads to neurological dysfunction),
- thiamin-responsive megaloblastic anemia (which involves genetic mutations that impair intestinal thiamin uptake and can lead to diabetes, megaloblastic anemia, cardiac impairments, and deafness), and
- biotin-thiamin responsive basal ganglia disease (which involves a recessive genetic mutation that causes thiamin transporter-2 deficiency, and can lead to ataxia, seizures, and encephalopathy).
Didn’t know vitamin B1 was this amazing? Maybe your friends will enjoy this too!
What are the Health Effects of Vitamin B1 (Thiamin) Deficiency?
Severe thiamin deficiency causes a disease called beriberi, which has been documented as far back as 2600 B.C. (when it was first described in Chinese literature). It’s derived from a Sinhalese phrase meaning “weak, weak” or “I cannot, I cannot”—referring to its damaging effects on nerve and muscular function. Beriberi impacts a number of systems in the body, particularly the central and peripheral nervous system, the cardiovascular system, and the GI tract.
Depending on which body systems the thiamin deficiency affects, beriberi has different subcategories.
- Wet beriberi affects the cardiovascular system (causing symptoms like leg swelling, enlarged heart, shortness of breath, rapid heart rate, and eventually congestive heart failure).
- Dry beriberi affects the nervous system (causing symptoms like neuropathy, numb hands and feet, difficulty moving the legs, pain, muscle atrophy, and abnormal reflexes), and in some cases causes a condition called Wernicke’s encephalopathy (characterized by biochemical lesions that result in confusion, loss of body movement control, and weakness or paralysis of eye muscles—and if left untreated, progresses to a chronic memory loss disorder called Korsakoff psychosis). These conditions are sometimes collectively referred to as Wernicke-Korsakoff syndrome.
- Gastrointestinal beriberi affects the gastrointestinal tract (due to thiamin deficiency limiting some stages of the Krebs cycle, pyruvate and lactate can accumulate and cause lactic acidosis—leading to nausea, severe abdominal pain, and vomiting).
- Infantile beriberi is sometimes seen in infants between two and six months old whose mothers don’t consume enough thiamin. Symptoms here include diarrhea, vomiting, edema, rapid heart rate, pale skin, edema, weight loss, and hoarseness when trying to cry or moan.
Along with inadequate dietary intake, thiamin deficiency can be caused by diseases that impair intestinal absorption, use of diuretics (particularly furosemide, which is often used to treat fluid retention from medical conditions like heart failure and liver disease), being on hemodialysis, anorexia, bariatric surgery, times of higher metabolic requirements (such has during pregnancy, breastfeeding, fever, strenuous exercise, and adolescent growth), and chronic alcoholism (in fact, alcohol abuse is the biggest cause of thiamin deficiency in industrialized areas, and makes people particularly susceptible to Wernicke’s encephalopathy and Korsakoff psychosis). Some infections, such as malaria, can also raise the risk of thiamin deficiency due to increasing the body’s metabolic demand for glucose (in turn requiring more thiamin-dependent enzyme activity related to glucose metabolism). HIV/AIDS patients are also at greater risk of thiamin deficiency due to increased thiamin needs. Some drugs, including the anticonvulsant medication phenytoin and the chemotherapy agent 5-fluorouracil, can also interfere with thiamin utilization, leading to reduced blood levels of thiamin or inhibiting the phosphorylation of thiamin to its active coenzyme form. And, obesity appears to increase the risk of thiamin deficiency, although the mechanisms aren’t fully understood.
Some foods also contain anti-thiamin factors (such as mycotoxins and thiaminases) that react with thiamin to form biologically inactive products that the body can no longer use. In particular, tea, coffee, and betel nuts contain heat-stable thiamin antagonists that can contribute to deficiency if consumed in large quantities, and freshwater fish, shellfish, horsetail, and ferns contain thiaminases that break down the thiamin in food (although these enzymes are typically deactivated by heat, and therefore are mostly a concern when eaten raw). In parts of Nigeria where wild silkworms are a dietary protein source, a neurological syndrome called seasonal ataxia can occur, due to the thiaminase present in these insects.
Everything You Need to Jump into Nutrivore TODAY!
Nutrivore Quickstart Guide
The Nutrivore Quickstart Guide e-book explains why and how to eat a Nutrivore diet, introduces the Nutrivore Score, gives a comprehensive tour of the full range of essential and important nutrients!
Plus, you’ll find the Top 100 Nutrivore Score Foods, analysis of food groups, practical tips to increase the nutrient density of your diet, and look-up tables for the Nutrivore Score of over 700 foods.
Buy now for instant digital access.
What are the Problems From Too Much Vitamin B1 (Thiamin)?
Thiamin supplements can sometimes cause unpleasant side effects such as nausea, tightness in the throat, rash, itching, and sweating or feeling too warm. These are more likely to occur when taking high-dose dietary supplements or injectable thiamin, rather than the lower oral doses contained in multivitamins (or from normal daily intakes of thiamin). Although more serious side effects are uncommon, be sure to seek medical advice from your healthcare provider if you’re considering supplementing with high doses of this micronutrient.
How Much Vitamin B1 (Thiamin) Do We Need?
The recommended dietary allowance (RDA) for thiamin is 1.1 mg per day for adult women (1.4 mg when pregnant or breastfeeding) and 1.2 mg per day for adult men. Although no tolerable upper intake level has been established (due to a general lack of toxicity from excess thiamin), in very rare cases, people have experienced anaphylactic reactions to large doses of intravenous thiamin.
| 0 – 6 months | |||||
| 6 months to < 12 months | |||||
| 1 yr – 3 yrs | |||||
| 4 yrs – 8 yrs | |||||
| 9 yrs – 13 yrs | |||||
| 14 yrs – 18 yrs | |||||
| 19 yrs – 50 yrs | |||||
| 51+ yrs | |||||
| Pregnant (14 – 18 yrs) | |||||
| Pregnant (19 – 30 yrs) | |||||
| Pregnant (31 – 50 yrs) | |||||
| Lactating (14 – 18 yrs) | |||||
| Lactating (19 – 30 yrs) | |||||
| Lactating (31 – 50 yrs) |
Nutrient Daily Values
Nutrition requirements and recommended nutrient intake for infants, children, adolescents, adults, mature adults, and pregnant and lactating individuals.
What are the Best Food Sources of Vitamin B1 (Thiamin)?
The following foods are the best sources of vitamin B1 (thiamin), containing 50% or more of the daily value per serving.
Want to know the top 500 most nutrient-dense foods?

Top 500 Nutrivore Foods
The Top 500 Nutrivore Foods e-book is an amazing reference deck of the top 500 most nutrient-dense foods according to their Nutrivore Score. Think of it as the go-to resource for a super-nerd, to learn more and better understand which foods stand out, and why!
If you are looking for a quick-reference guide to help enhance your diet with nutrients, and dive into the details of your favorite foods, this book is your one-stop-shop!
Buy now for instant digital access.
What are the Good Food Sources of Vitamin B1 (Thiamin)
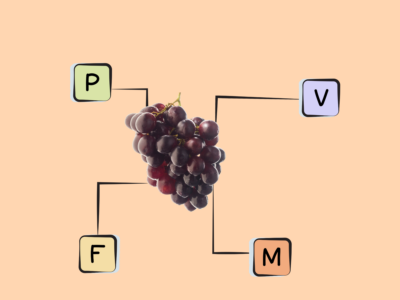
The following foods are also excellent or good sources of vitamin B1 (thiamin), containing at least 10% (and up to 20%) of the daily value per serving.
Nutrivore Is a Game-Changer—This FREE Guide Shows You Why
Sign up for the free Nutrivore Newsletter, your weekly, science-backed guide to improving health through nutrient-rich foods — without dieting harder —and get the Beginner’s Guide to Nutrivore delivered straight to your inbox!

Citations
Expand to see all scientific references for this article.
Alaei Shahmiri F, Soares MJ, Zhao Y, Sherriff J. High-dose thiamin supplementation improves glucose tolerance in hyperglycemic individuals: a randomized, double-blind cross-over trial. Eur J Nutr. 2013 Oct;52(7):1821-4. doi: 10.1007/s00394-013-0534-6.
Anwar A, Ahmed Azmi M, Siddiqui JA, Panhwar G, Shaikh F, Ariff M. Thiamin Level in Type I and Type II Diabetes Mellitus Patients: A Comparative Study Focusing on Hematological and Biochemical Evaluations. Cureus. 2020 May 8;12(5):e8027. doi: 10.7759/cureus.8027.
Bock CH, Ruterbusch JJ, Holowatyj AN, Steck SE, Van Dyke AL, Ho WJ, Cote ML, Hofmann JN, Davis F, Graubard BI, Schwartz KL, Purdue MP. Renal cell carcinoma risk associated with lower intake of micronutrients. Cancer Med. 2018 Aug;7(8):4087-4097. doi: 10.1002/cam4.1639.
Boros LG. Population thiamin status and varying cancer rates between western, Asian and African countries. Anticancer Res. 2000 May-Jun;20(3B):2245-8.
Chandrakumar A, Bhardwaj A, ‘t Jong GW. Review of thiamin deficiency disorders: Wernicke encephalopathy and Korsakoff psychosis. J Basic Clin Physiol Pharmacol. 2018 Oct 2;30(2):153-162. doi: 10.1515/jbcpp-2018-0075.
Chuang DT, Chuang JL, Wynn RM. Lessons from genetic disorders of branched-chain amino acid metabolism. J Nutr. 2006 Jan;136(1 Suppl):243S-9S. doi: 10.1093/jn/136.1.243S.
Cumming RG, Mitchell P, Smith W. Diet and cataract: the Blue Mountains Eye Study. Ophthalmology. 2000 Mar;107(3):450-6. doi: 10.1016/s0161-6420(99)00024-x.
Donnino M. Gastrointestinal beriberi: a previously unrecognized syndrome. Ann Intern Med. 2004 Dec 7;141(11):898-9. doi: 10.7326/0003-4819-141-11-200412070-00035.
Donnino MW, Andersen LW, Chase M, Berg KM, Tidswell M, Giberson T, Wolfe R, Moskowitz A, Smithline H, Ngo L, Cocchi MN; Center for Resuscitation Science Research Group. Randomized, Double-Blind, Placebo-Controlled Trial of Thiamin as a Metabolic Resuscitator in Septic Shock: A Pilot Study. Crit Care Med. 2016 Feb;44(2):360-7. doi: 10.1097/CCM.0000000000001572.
Doss A, Mahad D, Romanowski CA. Wernicke encephalopathy: unusual findings in nonalcoholic patients. J Comput Assist Tomogr. 2003 Mar-Apr;27(2):235-40. doi: 10.1097/00004728-200303000-00022.
Foulon V, Antonenkov VD, Croes K, Waelkens E, Mannaerts GP, Van Veldhoven PP, Casteels M. Purification, molecular cloning, and expression of 2-hydroxyphytanoyl-CoA lyase, a peroxisomal thiamin pyrophosphate-dependent enzyme that catalyzes the carbon-carbon bond cleavage during alpha-oxidation of 3-methyl-branched fatty acids. Proc Natl Acad Sci U S A. 1999 Aug 31;96(18):10039-44. doi: 10.1073/pnas.96.18.10039.
Gibson GE, Hirsch JA, Cirio RT, Jordan BD, Fonzetti P, Elder J. Abnormal thiamin-dependent processes in Alzheimer’s Disease. Lessons from diabetes. Mol Cell Neurosci. 2013 Jul;55:17-25. doi: 10.1016/j.mcn.2012.09.001.
Glasø M, Nordbø G, Diep L, Bøhmer T. Reduced concentrations of several vitamins in normal weight patients with late-onset dementia of the Alzheimer type without vascular disease. J Nutr Health Aging. 2004;8(5):407-13.
González-Ortiz M, Martínez-Abundis E, Robles-Cervantes JA, Ramírez-Ramírez V, Ramos-Zavala MG. Effect of thiamin administration on metabolic profile, cytokines and inflammatory markers in drug-naïve patients with type 2 diabetes. Eur J Nutr. 2011 Mar;50(2):145-9. doi: 10.1007/s00394-010-0123-x.
Harper C. Thiamin (vitamin B1) deficiency and associated brain damage is still common throughout the world and prevention is simple and safe! Eur J Neurol. 2006 Oct;13(10):1078-82. doi: 10.1111/j.1468-1331.2006.01530.x.
Hazell AS, Faim S, Wertheimer G, Silva VR, Marques CS. The impact of oxidative stress in thiamin deficiency: a multifactorial targeting issue. Neurochem Int. 2013 Apr;62(5):796-802. doi: 10.1016/j.neuint.2013.01.009.
Hiffler L, Rakotoambinina B, Lafferty N, Martinez Garcia D. Thiamin Deficiency in Tropical Pediatrics: New Insights into a Neglected but Vital Metabolic Challenge. Front Nutr. 2016 Jun 14;3:16. doi: 10.3389/fnut.2016.00016.
Institute of Medicine (US) Standing Committee on the Scientific Evaluation of Dietary Reference Intakes and its Panel on Folate, Other B Vitamins, and Choline. Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. Washington (DC): National Academies Press (US); 1998.
Jacques PF, Taylor A, Moeller S, Hankinson SE, Rogers G, Tung W, Ludovico J, Willett WC, Chylack LT Jr. Long-term nutrient intake and 5-year change in nuclear lens opacities. Arch Ophthalmol. 2005 Apr;123(4):517-26. doi: 10.1001/archopht.123.4.517.
Karuppagounder SS, Xu H, Shi Q, Chen LH, Pedrini S, Pechman D, Baker H, Beal MF, Gandy SE, Gibson GE. Thiamin deficiency induces oxidative stress and exacerbates the plaque pathology in Alzheimer’s mouse model. Neurobiol Aging. 2009 Oct;30(10):1587-600. doi: 10.1016/j.neurobiolaging.2007.12.013.
Krishna S, Taylor AM, Supanaranond W, Pukrittayakamee S, ter Kuile F, Tawfiq KM, Holloway PA, White NJ. Thiamin deficiency and malaria in adults from southeast Asia. Lancet. 1999 Feb 13;353(9152):546-9. doi: 10.1016/s0140-6736(98)06316-8.
Labay V, Raz T, Baron D, Mandel H, Williams H, Barrett T, Szargel R, McDonald L, Shalata A, Nosaka K, Gregory S, Cohen N. Mutations in SLC19A2 cause thiamin-responsive megaloblastic anaemia associated with diabetes mellitus and deafness. Nat Genet. 1999 Jul;22(3):300-4. doi: 10.1038/10372.
Lu’o’ng KV, Nguyễn LT. The role of thiamin in cancer: possible genetic and cellular signaling mechanisms. Cancer Genomics Proteomics. 2013 Jul-Aug;10(4):169-85.
Maguire D, Talwar D, Shiels PG, McMillan D. The role of thiamine dependent enzymes in obesity and obesity related chronic disease states: A systematic review. Clin Nutr ESPEN. 2018 Jun;25:8-17. doi: 10.1016/j.clnesp.2018.02.007.
Marik PE, Khangoora V, Rivera R, Hooper MH, Catravas J. Hydrocortisone, Vitamin C, and Thiamin for the Treatment of Severe Sepsis and Septic Shock: A Retrospective Before-After Study. Chest. 2017 Jun;151(6):1229-1238. doi: 10.1016/j.chest.2016.11.036.
Meador K, Loring D, Nichols M, Zamrini E, Rivner M, Posas H, Thompson E, Moore E. Preliminary findings of high-dose thiamin in dementia of Alzheimer’s type. J Geriatr Psychiatry Neurol. 1993 Oct-Dec;6(4):222-9. doi: 10.1177/089198879300600408.
Moskowitz A, Donnino MW. Thiamin (vitamin B1) in septic shock: a targeted therapy. J Thorac Dis. 2020 Feb;12(Suppl 1):S78-S83. doi: 10.21037/jtd.2019.12.82.
Müri RM, Von Overbeck J, Furrer J, Ballmer PE. Thiamin deficiency in HIV-positive patients: evaluation by erythrocyte transketolase activity and thiamin pyrophosphate effect. Clin Nutr. 1999 Dec;18(6):375-8. doi: 10.1016/s0261-5614(99)80019-3.
Nolan KA, Black RS, Sheu KF, Langberg J, Blass JP. A trial of thiamin in Alzheimer’s disease. Arch Neurol. 1991 Jan;48(1):81-3. doi: 10.1001/archneur.1991.00530130093025.
Polegato BF, Pereira AG, Azevedo PS, Costa NA, Zornoff LAM, Paiva SAR, Minicucci MF. Role of Thiamin in Health and Disease. Nutr Clin Pract. 2019 Aug;34(4):558-564. doi: 10.1002/ncp.10234.
Rodríguez-Martín JL, Qizilbash N, López-Arrieta JM. Thiamin for Alzheimer’s disease. Cochrane Database Syst Rev. 2001;(2):CD001498. doi: 10.1002/14651858.CD001498.
Stanga Z, Brunner A, Leuenberger M, Grimble RF, Shenkin A, Allison SP, Lobo DN. Nutrition in clinical practice-the refeeding syndrome: illustrative cases and guidelines for prevention and treatment. Eur J Clin Nutr. 2008 Jun;62(6):687-94. doi: 10.1038/sj.ejcn.1602854.
Suter PM, Haller J, Hany A, Vetter W. Diuretic use: a risk for subclinical thiamin deficiency in elderly patients. J Nutr Health Aging. 2000;4(2):69-71.
Thiamin: Fact Sheet for Health Professionals. National Institutes of Health (NIH) Office of Dietary Supplements. 26 Mar 2021.
Thornalley PJ, Babaei-Jadidi R, Al Ali H, Rabbani N, Antonysunil A, Larkin J, Ahmed A, Rayman G, Bodmer CW. High prevalence of low plasma thiamin concentration in diabetes linked to a marker of vascular disease. Diabetologia. 2007 Oct;50(10):2164-70. doi: 10.1007/s00125-007-0771-4.
Tylicki A, Siemieniuk M. Tiamina i jej pochodne w regulacji metabolizmu komórek [Thiamin and its derivatives in the regulation of cell metabolism]. Postepy Hig Med Dosw (Online). 2011 Jul 6;65:447-69. Polish. doi: 10.5604/17322693.951633.
Wang C, Fei G, Pan X, Sang S, Wang L, Zhong C, Jin L. High thiamin diphosphate level as a protective factor for Alzheimer’s disease. Neurol Res. 2018 Aug;40(8):658-665. doi: 10.1080/01616412.2018.1460704.
Whitfield KC, Bourassa MW, Adamolekun B, Bergeron G, Bettendorff L, Brown KH, Cox L, Fattal-Valevski A, Fischer PR, Frank EL, Hiffler L, Hlaing LM, Jefferds ME, Kapner H, Kounnavong S, Mousavi MPS, Roth DE, Tsaloglou MN, Wieringa F, Combs GF Jr. Thiamin deficiency disorders: diagnosis, prevalence, and a roadmap for global control programs. Ann N Y Acad Sci. 2018 Oct;1430(1):3-43. doi: 10.1111/nyas.13919.
Yamasaki H, Tada H, Kawano S, Aonuma K. Reversible pulmonary hypertension, lactic acidosis, and rapidly evolving multiple organ failure as manifestations of shoshin beriberi. Circ J. 2010 Sep;74(9):1983-5. doi: 10.1253/circj.cj-10-0202.
Zastre JA, Hanberry BS, Sweet RL, McGinnis AC, Venuti KR, Bartlett MG, Govindarajan R. Up-regulation of vitamin B1 homeostasis genes in breast cancer. J Nutr Biochem. 2013 Sep;24(9):1616-24. doi: 10.1016/j.jnutbio.2013.02.002.