A stroke occurs when blood flow to a portion of the brain is interrupted, either due to a blocked artery (ischemic stroke) or the rupture of a blood vessel (hemorrhagic stroke). When the brain is deprived of oxygen-rich blood, brain cells in the affected area begin to die, resulting in potential long-term disabilities such as speech impairment, paralysis, and cognitive deficits. Strokes can have sudden and life-altering consequences, and immediate medical attention is crucial to reduce the extent of damage.
Each year, approximately 795,000 people in the U.S. experience a stroke, according to the CDC. Stroke is the fifth leading cause of death in the U.S. and a leading cause of severe, long-term disability among adults.
A stroke, also known as a cerebrovascular accident (CVA), is a serious medical emergency that occurs when the blood supply to a part of the brain is disrupted, causing brain cells to be deprived of oxygen and nutrients. When this happens, brain cells begin to die within minutes, potentially leading to lasting brain damage, disability, or even death. Stroke is a leading cause of death and long-term disability worldwide, but many strokes are preventable, and the effects can often be minimized with prompt treatment.
There are three types of strokes:
- Ischemic Stroke: This is the most common type, accounting for about 87% of all strokes. It occurs when a blood clot or other obstruction (such as a fatty deposit) blocks the blood flow in an artery supplying the brain. This blockage prevents oxygenated blood from reaching the affected brain tissue, causing damage or death to brain cells.
- Hemorrhagic Stroke: This type occurs when a blood vessel in the brain bursts, leading to bleeding in or around the brain. The leaking blood creates pressure on the brain cells, damaging them. Hemorrhagic strokes are typically caused by conditions like high blood pressure or aneurysms (weakened blood vessels that burst).
- Transient Ischemic Attack (TIA): A third, less severe type of stroke, and is also commonly known as a “mini stroke.” A TIA occurs when there is a temporary disruption in blood flow to the brain, usually lasting only a few minutes. Though it does not cause permanent damage, a TIA serves as a warning sign of a future stroke and should never be ignored.
What Are Causes and Risk Factors of Stroke?
The underlying cause of a stroke is either a blocked or ruptured blood vessel, but several factors contribute to the conditions that lead to these events.
- Atherosclerosis: This condition involves the buildup of fatty deposits (plaque) in the arteries. Plaque can harden or rupture, causing blood clots that obstruct blood flow to the brain, leading to an ischemic stroke.
- Blood Clots: Clots can form in the heart, especially in individuals with certain heart conditions like atrial fibrillation (irregular heartbeat). These clots can travel to the brain and block blood flow, causing a stroke.
- High Blood Pressure (Hypertension): Chronic high blood pressure weakens the walls of blood vessels, making them more prone to rupture, which can lead to a hemorrhagic stroke. Hypertension is one of the most significant risk factors for stroke.
- Aneurysms: An aneurysm is a weakened area of a blood vessel that can bulge and potentially burst, leading to a hemorrhagic stroke. High blood pressure and certain genetic factors increase the risk of developing an aneurysm.
- Heart Disease: Conditions like atrial fibrillation, coronary artery disease, and heart failure can increase the risk of stroke by contributing to the formation of blood clots or decreasing overall blood flow to the brain.
- Injuries or Trauma: A traumatic injury to the head can cause blood vessels in the brain to rupture, leading to a hemorrhagic stroke.
- Age: The risk of stroke increases with age. People over the age of 55 have a higher likelihood of experiencing a stroke, though it can happen at any age.
- Gender: While men are at higher risk of having a stroke at a younger age, women tend to live longer, and strokes are more likely to be fatal in women. Additionally, certain risk factors, like pregnancy, use of birth control pills, and hormone replacement therapy, can increase the risk of stroke in women.
- Family History: If a close relative has had a stroke, the risk of having a stroke increases, particularly due to genetic factors that may contribute to conditions like high blood pressure or diabetes.
- Ethnicity: African Americans, Hispanics, and Native Americans are at higher risk of stroke than other ethnic groups, largely due to a higher prevalence of hypertension, diabetes, and obesity.
- High Blood Pressure: Chronic hypertension is the leading risk factor for stroke. It damages blood vessels over time, making them more susceptible to rupture or blockage.
- Diabetes: Diabetes increases the risk of stroke because high blood sugar levels can damage blood vessels and contribute to the formation of clots.
- Smoking: Smoking significantly increases the risk of stroke by damaging the blood vessels and promoting the buildup of plaque. It also increases the likelihood of forming blood clots.
- High Cholesterol: High levels of cholesterol contribute to the buildup of plaque in the arteries, increasing the risk of an ischemic stroke.
- Sedentary Lifestyle and Obesity: Lack of regular physical activity and being overweight or obese are significant risk factors for stroke, as they contribute to hypertension, diabetes, and heart disease.
How Do You Reduce Risk of Stroke

While some risk factors, like age and genetics, cannot be changed, many strokes can be prevented through healthy lifestyle choices and managing underlying health conditions.
- Control Blood Pressure: Maintaining healthy blood pressure is crucial in reducing the risk of both ischemic and hemorrhagic strokes. Lifestyle changes, such as reducing salt intake, exercising regularly, and managing stress, can help lower blood pressure. In some cases, medication may be necessary to keep blood pressure under control.
- Manage Diabetes: Keeping blood sugar levels within a healthy range is essential for reducing the risk of stroke. This can be achieved through a combination of a healthy diet, regular physical activity, and medication when necessary.
- Adopt a Nutrivore Diet: Eating a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats (such as those from nuts and fish) can help lower cholesterol, blood pressure, and blood sugar, reducing the risk of stroke.
- Quit Smoking: Smoking cessation is one of the most effective ways to reduce the risk of stroke. Within a few years of quitting, a former smoker’s stroke risk decreases significantly.
- Exercise Regularly: Regular physical activity helps improve overall cardiovascular health, lower blood pressure, reduce cholesterol levels, and maintain a healthy weight—all of which contribute to stroke prevention.
- Limit Alcohol Intake: Drinking alcohol in moderation, or not at all, can help reduce the risk of high blood pressure and, consequently, stroke.
Nutrients for Stroke
Learn more about all of the nutrients linked to risk of stroke, the other ways these nutrients improve our health, and the best food sources of each of them!
How Do Nutrients Improve Stroke?
A Nutrivore approach emphasizes nutrients that help the body function at its best, including the pathways that support healthy arteries, circulation, and brain function. Current research highlights the following nutrients for stroke, along with food sources to help you incorporate these nutrients through your diet.
| Nutrient | How it Supports Stroke Prevention or Recovery | Top Food Sources |
|---|---|---|
| Vitamin B2 (Riboflavin) | Low riboflavin intake is linked to increased stroke risk, particularly in people with the MTHFR C677T genetic variant due to impaired homocysteine metabolism; adequate intake may help reduce this risk. | Organ meats, mushrooms, leafy greens, eggs, dairy, almonds, yeast, legumes, and squash. |
| Vitamin B3 (Niacin) | Higher niacin intake is associated with lower stroke mortality, and supplementation reduces inflammation and improves lipid metabolism, both important for lowering stroke risk. | Red meat, poultry, seafood like salmon and tuna, yeast, organ meat, shellfish, mushrooms, leafy greens, nuts, seeds, legumes, and fortified grains. |
| Vitamin B6 | Higher vitamin B6 status is associated with reduced stroke risk, potentially due to its role in homocysteine regulation and vascular health. | Fish, leafy greens, root vegetables, bananas, chickpeas, red meat, poultry, seeds, and fortified cereals. |
| Vitamin B9 (Folate) | Folate lowers homocysteine levels and significantly reduces stroke risk, especially in populations without folic-acid–fortified foods; supplementation lowers first-ever stroke incidence. | Liver, leafy greens, asparagus, avocados, Brussels sprouts, legumes, eggs, beets, citrus fruits, strawberries, pomegranates, broccoli, nuts, seeds, and fortified grains. |
| Vitamin B12 | Low B12 status increases homocysteine levels and is linked with higher risk of ischemic stroke; combined folate + B12 supplementation reduces stroke incidence more effectively than folate alone. | Fish, shellfish, organ meats, beef, eggs, poultry, dairy, tempeh, and fortified cereals or plant milks. |
| Vitamin C | Higher vitamin C intake is associated with lower stroke risk, and higher plasma vitamin C is linked with reduced cardiovascular mortality and improved endothelial health. | Citrus fruits, kiwis, berries, red peppers, guavas, papayas, broccoli, Brussels sprouts, tomatoes, cantaloupe, leafy greens, and certain organ meats. |
| Vitamin D | Low vitamin D is linked with higher stroke incidence and severity; adequate levels may support vascular function and blood-pressure regulation, both important for reducing stroke risk. | Fatty fish, fish eggs, liver, red meat, egg yolks, and UV-exposed mushrooms or yeast. |
| Vitamin E | Vitamin E reduces oxidative stress and may help protect against ischemic stroke by lowering LDL oxidation and supporting vascular health, though supplementation trials show mixed results. | Sunflower seeds, almonds, hazelnuts, avocados, olives/olive oil, palm oil, vegetable oils, fatty fish, organ meats, tomatoes, oats, wheat germ, peanuts, chestnuts, coconut, kiwis, carrots, and fortified cereals. |
| Vitamin K | Higher vitamin K intake is associated with lower cardiovascular mortality and may protect against arterial calcification, which contributes to stroke risk; observational data show reduced stroke incidence with higher intake. | Leafy greens (kale, chard, collards, spinach), broccoli, Brussels sprouts (K1); natto, liver, egg yolks, hard cheeses, butter, pork, and dark chicken meat (K2). |
| Calcium | Adequate calcium intake is associated with lower stroke risk and lower blood pressure, though very high supplemental doses may increase cardiovascular event risk. Dietary calcium appears protective. | Dairy (including low-fat), bone-in sardines, Brassica vegetables, seaweed, beans, and calcium-fortified foods. |
| Chloride | In combination with sodium, chloride influences blood pressure regulation, and high sodium chloride intake increases stroke risk through vascular strain and hypertension, especially in salt-sensitive individuals. | Seafood such as prawns and salmon, seaweed, tomatoes, olives, celery, lettuce, and foods prepared with table salt. |
| Magnesium | Higher magnesium intake is strongly linked with lower stroke risk, especially ischemic stroke, likely through blood-pressure reduction, vascular relaxation, and anti-inflammatory effects. | Leafy greens, pumpkin seeds, almonds, cashews, fish, legumes, whole grains, cocoa, avocados, spices, and low-fat dairy. |
| Potassium | Potassium reduces stroke risk by lowering blood pressure, improving vascular function, and counteracting sodium’s harmful effects; higher intake consistently predicts lower stroke incidence. | Leafy greens, cruciferous vegetables, melons, bananas, apricots, plums, prunes, oranges/orange juice, potatoes, sweet potatoes, squash, avocados, mushrooms, legumes, nuts, seeds, and dairy. |
| Sodium | High sodium intake increases stroke risk by raising blood pressure, impairing vascular function, and promoting arterial stiffness; reductions in sodium intake decrease stroke incidence across populations. | Highest in processed and packaged foods, cured meats, salted snacks, pickles, olives, bread, fast food, canned foods, soy sauce, salad dressings; naturally in seafood, seaweed, vegetables like celery and chard, milk, and baking soda. |
| Zinc | Evidence suggests zinc may protect against atherosclerosis and oxidative stress, with lower zinc levels associated with higher stroke risk; supplementation may support vascular repair. | Red meat, liver, heart, oysters, eggs, legumes, nuts, and whole grains (with higher absorption from animal foods). |
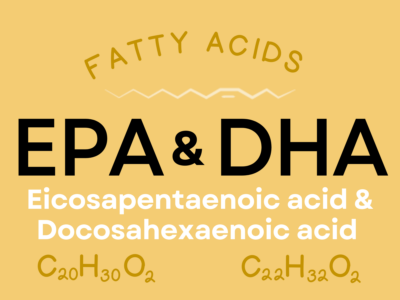
| Omega-3s (EPA & DHA) | EPA and DHA reduce blood pressure, lower triglycerides, stabilize heart rhythm, reduce inflammation, and may significantly reduce fatal stroke events and ischemic stroke risk. | Salmon, herring, mackerel, sardines, menhaden, marine algae, cod liver oil, mussels, crab, oysters, and squid. |
| Oleic Acid | Oleic acid improves lipid profiles, reduces inflammation, and enhances endothelial function; higher intake is linked with reduced stroke risk in Mediterranean populations. | Olives/olive oil, avocados/avocado oil, nuts, seeds, and vegetable oils including peanut, canola, sunflower, sesame, grapeseed, and soybean; cocoa butter and some animal fats also contain oleic acid. |
| SCFAs | SCFAs may reduce stroke severity by preserving blood–brain barrier integrity and reducing inflammation; early research shows SCFAs can improve neurological recovery after ischemic stroke. | Butter/high-fat dairy, lacto-fermented foods (yogurt, sauerkraut, pickles, soy sauce, certain cheeses), vinegar, alcohol; most SCFAs come from microbial fermentation of fiber. |
Nutrients for Stroke
Nutrients for Stroke explains all the nutrients that matter most for stroke risk and brain health! This e-book is exclusively available in Patreon!
Plus every month, you’ll gain exclusive and early access to a variety of resources, including a weekly video podcast, a new e-book in a series, nutrient fun factsheet, and more! Sign up now and also get 5 free Nutrivore guides as a welcome gift! Win-win-win!
Benefits of a Food-Based Approach

A nutrient-focused, whole-food approach can play a supportive role in managing many health conditions, especially when paired with healthy lifestyle habits like physical activity and good-quality sleep. A food-based approach to nutrition offers health benefits that go far beyond what supplements can provide. Whole foods deliver a natural balance of nutrients that work synergistically, meaning vitamins, minerals, phytonutrients, healthy fats, carbohydrates and fiber can support each other for better overall health outcomes. Nutrient-dense foods like leafy greens, fruits, legumes, nuts, seeds, and fish are efficient, cost-effective, and widely accessible options that fit easily into a healthy diet and good eating patterns. By choosing whole foods first, you not only support a more balanced diet but also avoid the added costs and potential nutrient insufficiencies that can come with eating highly processed foods and relying solely on supplements to make up the shortfall.
The variety of nutrient-dense foods available across food groups makes it easy to enjoy a satisfying, diverse, and plant-forward (though not solely plant-based) way of eating. Many of these foods provide additional health benefits including antioxidants (which are anti-inflammatory), insoluble fiber for gut health, which in turn supports overall health and wellness. Because whole foods are often more accessible and affordable than supplements, a food-based approach creates a sustainable foundation for long-term well-being.
Nutrivore encourages filling your plate with a wide range of nutrient-rich foods without the need for restrictive rules, making it easy to prevent and support health conditions through the simple power of food. With a Nutrivore approach (maximizing nutrient density across food groups), a nutritious, balanced, and enjoyable way of eating becomes both achievable and flexible for any lifestyle. While it isn’t a replacement for medical care or the advice of a registered dietitian, a balanced, food-first approach can complement your overall strategy for improving many health conditions and support long-term health goals.