Key Takeaways (expand)
- Despite its often negative health reputation, sodium is an essential mineral that’s needed for life.
- As an electrolyte, sodium has a major role in regulating blood pressure and blood volume, largely via the renin-angiotensin-aldosterone system (which governs sodium and potassium retention and excretion) and the pituitary gland (which adjusts sodium and water resorption in response to drops in blood pressure or volume).
- Sodium works in conjunction with potassium to create a gradient of electrical charge called the membrane potential, which then helps control a number of life-sustaining processes including heart function, muscle contraction, and the transmission of nerve impulses.
- Sodium intake has been observationally linked to higher blood pressure, and subsequently to an increased risk of hypertension-related disorders like cardiovascular disease, chronic renal failure, hypertensive retinopathy, and even diabetes.
- The true effect of sodium on blood pressure is more nuanced than often portrayed: there’s significant individual variation in people’s sodium sensitivity, with “salt sensitive” individuals seeing their blood pressure rise in response to sodium intake, while “salt resistant” individuals see little to no change in blood pressure under the same conditions.
- Likewise, the dietary ratio of sodium to potassium may be more important than sodium intake alone, as higher potassium appears to counteract the negative effects of sodium on blood pressure and endothelial function.
- Controlled studies looking at sodium intake and health outcomes haven’t confirmed the correlations seen in observational studies, and generally fail to show that sodium restriction protects against cardiovascular events or mortality.
- Some evidence suggests excess sodium can promote osteoporosis, due to increasing calcium excretion in the urine; consuming higher amounts of calcium and/or potassium may help protect against this effect.
- Sodium-induced increases in urinary calcium could also raise the risk of kidney stones.
- Excess sodium can potentially worsen existing kidney disease, both due to direct tissue damage from sodium and due to an altered gradient of sodium concentration impairing kidney function.
- High sodium intakes have an immune-stimulating effect (activating macrophages and potentially promoting inflammation), and some limited evidence suggests this could contribute to autoimmunity and asthma.
- Observational research has linked excess sodium to a higher risk of stomach cancer, possibly by damaging the mucosal cells of the stomach, increasing the infection risk and virulence of H. pylori (a major risk factor for ulcers and stomach cancer), and increasing the stomach’s exposure to gastric carcinogens.
- Very low sodium intake can also be a health risk, with studies linking low-sodium diets to increases in adrenaline, LDL cholesterol, triglycerides, insulin resistance, risk of end-stage renal disease among diabetics, and total mortality.
- Sodium deficiency rarely happens due to inadequate intake, but blood levels can drop too low in response to illness (extended vomiting or diarrhea), chronic disease (especially kidney, liver, or heart disease), certain medications, or fluid overload during exercise; when this occurs, the condition is known as hyponatremia.
- Long-term hyponatremia is associated with significantly higher mortality risk, and can produce symptoms such as confusion, lethargy, altered personality, nausea, and vomiting.
- Sodium naturally occurs in seaweed, seafood, spinach, chard, celery, beets, carrots, and milk, although most people get abundant amounts through foods with salt added during cooking or processing.
Table of Contents[Hide][Show]
Although sodium often gets a bad rap, it’s actually an essential mineral needed for life! It was first isolated in 1807 by English chemist Sir Humphry Davy, who also isolated calcium, potassium, barium, strontium, boron, and magnesium. However, sodium—in the form of sodium chloride (NaCL), better known as table salt—has been mined and cherished for thousands of years, and was once considered so valuable that Roman legions were paid with it (hence the word salary, which comes from the word salt!). We could even argue that salt made modern civilization possible: it gave us the ability to preserve food without refrigeration, allowing us to store and trade perishable items, prevent meat from rotting, travel long distances with a secure food supply, and release our dependence on seasonal eating.
Importantly, this nutrient functions as an electrolyte—a class of minerals that dissociate into charged particles (called ions) when dissolved in solution, making them capable of conducting electricity. On the whole, electrolytes help regulate fluid balance within the body, regulate nerve and muscle function (including the heart!), maintain a normal blood pH, and transmit nerve signals!
Sodium is ubiquitous in most diets due to the addition of table salt (sodium chloride) during cooking and processing, with the highest sources being soup, cured meats, salted nuts and seeds, pickles, olives, bread, packaged snacks (like chips and pretzels), fast food meals, and canned foods. A number of condiments, such as soy sauce and salad dressings, also have a very high sodium content. Sources of naturally-occurring sodium include some seafood (especially lobster, crab, mussels, clams, shrimp, scallops, oysters, and octopus), seaweed, fish eggs, spinach, celery, chard, beets, carrots, and milk. Baking soda, or sodium bicarbonate, is also very high in sodium.
The Biological Roles of Sodium
One of sodium’s most important roles is in blood pressure regulation and blood volume. In fact, a number of mechanisms control blood pressure and blood volume specifically by adjusting sodium levels within the body! One of the major ways this is done is via the renin-angiotensin-aldosterone system. In order to keep track of body water loss, osmoreceptors in the hypothalamus sense changes in water concentration and sodium balance in extracellular fluids (such as blood plasma, joint fluid, cerebrospinal fluid, and the fluid between cells—called interstitial fluid). When a significant drop in blood volume or pressure is detected (such as from dehydration or blood loss), the kidneys respond by releasing an enzyme called renin into circulation. Renin splits a protein called angiotensinogen into a smaller peptide called angiotensin I, which then gets split even further into angiotensin II by the angiotensin converting enzyme (ACE), which is found in the lungs, kidneys, liver, and the inner surface of blood vessels. Along with increasing blood pressure by inducing small artery constriction, angiotensin II prompts the adrenal glands to synthesize aldosterone—a steroid hormone that directs the kidneys to excrete more potassium and retain more sodium. As a result of this increased sodium retention, less urine gets produced, blood volume increases, and blood pressure rises.
The pituitary gland also plays a role in sodium and fluid balance. When blood pressure or blood volume significantly drop, the posterior pituitary gland secretes vasopressin (sometimes also called anti-diuretic hormone, or ADH). Vasopressin then stimulates epithelial sodium channels to increase the reabsorption of sodium and water, leading to higher fluid levels in the body and a restoration of blood pressure. Conversely, when sodium concentrations get too low (such as from drinking a very large amount of water), the pituitary gland decreases the amount of vasopressin being secreted, resulting in more water loss through urine and consequently, an increase in relative sodium concentrations.
Potassium is the main positively charged ion within cells, while sodium is the main positively charged ion outside of cells. The concentration differences between these two minerals is called the membrane potential, and it creates a gradient with an electrical charge that directs the flow of ions (with positively charged ions moving towards the negatively charged side of the membrane, and negatively charged ions moving towards the positively charged side of the membrane). The membrane potential is maintained by ion pumps located within the cell membrane, which use ATP to pump sodium out in exchange for potassium—ultimately allowing for the control of muscle contraction, heart function, and the transmission of nerve impulses. In fact, because it plays such an important role in sustaining life, the body dedicates an enormous amount of energy to regulating the membrane potential: the activity of ion pumps accounts for about 20-40% of our total resting energy expenditure each day!
Sodium and chloride have a close relationship with each other when it comes to controlling blood pressure and extracellular fluid volume. Urinary secretion of sodium and chloride are closely correlated, and chloride enables the reabsorption of sodium filtered from the urinary tubules into extracellular spaces in the body. Both of these minerals are involved in the renin-angiotensin-aldosterone system, with chloride concentration inversely regulating renin secretion, and renin secretion ultimately dictating how much sodium and water gets retained. In addition, because sodium and chloride are so commonly consumed together (in the form of table salt), it’s sometimes difficult to scientifically assess the individual effects of sodium versus chloride!
Everything You Need to Jump into Nutrivore TODAY!
Nutrivore Quickstart Guide
The Nutrivore Quickstart Guide e-book explains why and how to eat a Nutrivore diet, introduces the Nutrivore Score, gives a comprehensive tour of the full range of essential and important nutrients!
Plus, you’ll find the Top 100 Nutrivore Score Foods, analysis of food groups, practical tips to increase the nutrient density of your diet, and look-up tables for the Nutrivore Score of over 700 foods.
Buy now for instant digital access.
Problems From Too Much Sodium
A number of observational studies have linked excess sodium intake with higher blood pressure and blood-pressure-related conditions, including cardiovascular disease, chronic renal failure, diabetes, and hypertensive retinopathy. However, controlled trials generally don’t show a benefit of sodium restriction on actual health outcomes, and its blood-pressure-raising effects may be limited to people who are “salt sensitive” (that is, have an impaired ability to maintain sodium homeostasis). However, excess sodium—particularly in conjunction with low potassium and/or low calcium—could also increase the risk of osteoporosis and kidney stones, due to increasing the amount of calcium excreted in urine. High sodium intake could also potentially worsen kidney disease, contribute to stomach cancer risk, and increase the risk of asthma or autoimmunity.
Sodium, Hypertension and Cardiovascular Disease
Sodium has received plenty of attention for its contribution to high blood pressure—which itself is a risk factor for not only cardiovascular disease (including heart disease, heart attack, heart failure, and stroke), but also for hypertensive retinopathy, chronic renal failure, and even diabetes. A number of observational studies have indeed linked excess sodium intake with higher blood pressure, and some trials have shown that sodium reduction can prevent or improve hypertension (especially among groups of people who are at particularly high risk). For example, several multi-center trials found that decreasing sodium intake by about 1 g per day resulted better control of hypertension in older adults on medication, decreased systolic (but not diastolic) blood pressure in overweight participants with pre-hypertension, and reduced the risk of developing full-blown hypertension over the course of four years. A number of other randomized trials have tested the effects of sodium reduction on blood pressure in both healthy and hypertensive results, and have generally shown that reducing sodium intake by anywhere from 1.8 to 3.2 g daily reduces blood pressure in a dose-response fashion. However, this is mostly seen in people whose baseline blood pressure is over 130/80 mm Hg.
That being said, the effects of sodium on actual disease risk and mortality have been far less clear cut! On one hand, some studies show that high sodium intake can impair endothelial function (a risk factor for heart disease), giving sodium yet another potential mechanism for contributing to cardiovascular disease on top of its effects on blood pressure. And, some prospective cohort studies have found increased incidence of cardiovascular disease and stroke among people with higher versus lower sodium intake. However, controlled studies looking at health outcomes (rather than just risk factors) have generally failed to show that reducing sodium intake actually helps protect against cardiovascular disease or death. For example, a Cochrane review using eight different trials found that sodium restriction had no significant benefit for overall mortality, and only weak benefit for cardiovascular events and deaths. And, that benefit was due almost entirely to a single trial of retirement home residents, which drove the results when all eight studies were pooled together—meaning the vast majority of trials actually failed to show that reducing sodium actually improved health outcomes!
Part of the difficulty in drawing conclusions about sodium’s effect on heart disease risk is that sodium sensitivity varies dramatically among individuals. While some people are “salt sensitive” and respond to alterations in sodium intake with clear changes in blood pressure, others exhibit little to no change in blood pressure under the same circumstances (such people are called “salt resistant”). A person’s individual salt sensitivity or resistance is determined by their glomerular filtration rate (how much blood passes through tiny filters in the kidneys, called glomeruli) and how much sodium reabsorption occurs in their kidney’s proximal tubules (which contribute to fluid and electrolyte homeostasis). In all, about a quarter of people with normal blood pressure and half of people with high blood pressure are salt sensitive, and some research suggests that salt sensitivity may be more of a risk factor for cardiovascular disease than sodium intake alone. So, consuming more or less sodium won’t universally affect people in the same way.
Importantly, when it comes to health outcomes, the dietary sodium-to-potassium ratio also matters. Research points to a nutrient interaction in which higher sodium intake is mostly harmful in the presence of low potassium intake (as measured by excretion levels of both minerals); for example, adding potassium to a high-sodium meal is able to attenuate the sodium-induced endothelial dysfunction typically seen, and added potassium can reduce blood pressure even without a concurrent reduction in sodium intake. Similarly, some of the trials showing a benefit of sodium reduction on blood pressure (such as those using the famous Dietary Approaches to Stop Hypertension, or DASH diet) found that sodium reduction had an impact in the context of a standard Westernized diet, but not among participants eating a higher-potassium diet rich in vegetables, fruits, lean protein, and whole grains. So, the effects of sodium on cardiovascular health may be more nuanced than initially thought, and influenced by other factors like salt sensitivity and other dietary components.
Sodium and Bone Health
Some research suggests that a high sodium intake could also promote osteoporosis. Dietary sodium is known to increase the loss of calcium through the urine—possibly due to sodium and calcium competing for reabsorption in the kidneys, or through sodium’s effect on parathyroid hormone secretion (which in turn regulates calcium levels).
Observational studies have shown that markers of sodium intake are associated with lower bone mineral density in the hip, and that high sodium intake coupled with low calcium intake appears particularly detrimental for bone health. Meanwhile, a study of postmenopausal women found that as long as calcium intake was sufficient, habitually ingesting about 3 g per day of sodium didn’t decrease bone mineral density. Statistical analyses likewise estimate that lowering sodium intake to 2.3 g daily while boosting calcium intake to 1.2 g daily could prevent any sodium-induced loss of bone mineral density! A small controlled trial also found that potassium supplementation (in the form of potassium citrate) prevented the excess calcium loss usually seen with high sodium diets (in this case, 5 g of sodium per day), highlighting the importance of nutrient interactions when it comes to the sodium-skeletal health link.
Sodium and Kidney Health
High sodium intake has also been known to worsen existing kidney disease, and some evidence suggests it could increase the risk of developing kidney disease in the first place. This may be due to the kidneys’ role in maintaining fluid and electrolyte balance, as well as in the removal of water-soluble waste products from the body (which are excreted in urine). In the production of urine, the kidneys remove water from the blood via osmosis (meaning the water moves from an area of low concentration of electrolytes across a semi-permeable barrier of cells to an area of high concentration of electrolytes). A high-sodium diet alters the gradient of sodium concentration, causing the kidneys to have reduced function and remove less water, resulting in higher blood volume (and therefore pressure). Strain on the kidneys comes not just from hypertension and a reduced ability to perform its filtering job, but also from direct tissue damage from high sodium levels. However, contrary to what the sodium-kidney disease correlations would imply, reduced sodium diets don’t appear to improve the progression of chronic kidney disease in the long term, nor do they seem to reduce mortality. However, such diets do improve the response to several drug options for mitigating kidney disease, and are still a recommendable option for anyone battling established kidney problems.
Similarly, through its effect of increasing calcium excretion, sodium may raise the risk of kidney stones. Elevated urinary calcium levels (called hypercalciuria) is a risk factor for kidney stone formation, and large observational studies have shown that people with high average sodium intakes have a 30% greater risk of developing kidney stones over the course of 12 years, compared to people with lower sodium intakes. Likewise, in one trial, putting people with high baseline urinary calcium levels on a diet with low sodium and normal calcium (1.2 g daily of each) was able to reduce the recurrence of kidney stones by almost 50%, compared to a diet that was only low in calcium.
Sodium and Immunity
High sodium intake also stimulates the immune system, and some limited evidence suggests it may contribute to autoimmunity. For one, sodium intake has been shown to activate macrophages (resident immune cell sentinels present in nearly every tissue in the human body) and potentially promote inflammation.
One study found that the higher the concentration of sodium in the diet, the greater the number of Th17 cells (a major culprit in autoimmune disease) that are activated, and the greater the amount of proinflammatory cytokines that are secreted by those Th17 cells (causing generalized inflammation). In rodent models of multiple sclerosis, high-sodium diets have been shown to exacerbate symptoms due to increases in Th17 cell differentiation, proliferation, and activation; females appear particularly susceptible to this effect.
In humans, studies have shown that high dietary sodium intake increased risk of rheumatoid arthritis in smokers (but not non-smokers), and that asthmatics are more likely to have exercise-induced asthmatic attacks if they eat a high-sodium diet (while also seeing improvements in their symptoms when adopting a low-sodium diet).
However, more human studies are needed to explore the potential links between sodium and the immune system, especially in relation to the intake of other nutrients that sodium interacts with.
Sodium and Stomach Cancer
Some research also suggests that excess sodium may increase the risk of stomach cancer. For instance, a meta-analysis of seven prospective studies, encompassing almost 270,000 people, found that people with the highest intake of salt had a 68% greater risk of developing stomach cancer compared to people with the lowest intake of salt. Multiple observational studies have also linked high-sodium foods (such as pickled foods, processed meat products, and salted foods) with an increased risk of gastric cancer.
Although these links are associative, sodium does have multiple mechanisms by which it could plausibly contribute to the etiology of stomach cancer. For one, high sodium levels can damage the mucosal cells in the stomach, which in turn increases the risk of infection by H. pylori—a bacteria that grows in the intestinal tract, and which is a major risk factor for ulcers and stomach cancer. In addition, H. pylori reacts to high-salt environments with an increase in growth, cell morphology, survival, and virulence—all of which result in a more aggressive infection that becomes an even stronger promoter of stomach cancer. Some rodent studies also suggest that high-sodium diets can increase the carcinogenic effects of certain H. pylori strains by causing more severe stomach inflammation, raising the gastric pH, increasing the expression of interleukin 1β in gastric cells, and upregulating the synthesis of cytotoxin-associated gene A (a bacterial oncoprotein that can bind to proteins and deregulate them, thus potentially causing cancer).
Apart from the role of H. pylori, sodium can raise stomach cancer risk through two other avenues: increasing exposure to gastric carcinogens such as nitrates, and causing inflammation that leads to increased cell proliferation and mutation (which boosts the risk of cancer developing). This happens because a high sodium intake can alter the quality of the stomach’s mucous barrier, leading to direct exposure to harmful compounds and also making the stomach more susceptible to mucosal damage.
Hypernatremia
In rare cases (like drinking seawater), ingesting very high amounts of salt at one time can cause hypernatremia—a condition where sodium levels in the blood are elevated above 145 mM. This produces symptoms like vomiting, nausea, diarrhea, and abdominal cramps. Generally, the body is able to cope with a sodium influx by pulling water from cells and into extracellular fluid, so the risk of hypernatremia is mostly present when fluid needs can’t be met or when the kidneys aren’t functioning properly. More often, dangerously high blood sodium concentrations occur due to water loss rather than sodium intake—especially during severe burns, respiratory infections, osmotic diarrhea, or hypothalamic disorders.
Didn’t know sodium was this interesting? Maybe your friends will enjoy this too!
Problems from Low-Sodium Diets
Sodium restriction could pose some health risks of its own, including increasing LDL cholesterol, adrenaline, triglycerides, renal disease risk among diabetics, and even total mortality risk. Abnormally low blood levels of sodium, called hyponatremia, can also increase the risk of mortality and cause brain swelling, although this more often happens due to excess sodium excretion (such as due to infectious illness, chronic disease, or fluid overload during exercise) rather than inadequate intake.
Although the dangers of too much sodium receive plenty of attention, some evidence suggests that low-sodium diets could pose their own health risks. A Cochrane review drawing from 195 references found that while lowering sodium intake below 2.3 g daily generally reduced blood pressure, it also had adverse effects on hormones and blood lipids—including raising adrenaline, cholesterol (including LDL cholesterol), and triglycerides.
Some (but not all) studies have also found that low-sodium diets quickly induce insulin resistance and potentially raise the risk of diabetes—possibly due to the activating effects of reduced sodium on the renin-angiotensin-aldosterone system and sympathetic nervous system, both of which can contribute insulin resistance. In fact, several observational studies found low sodium intake to be associated with an increased risk of end-stage renal disease and death among people with type 1 and type 2 diabetes (although other studies have found neutral or beneficial effects of sodium on insulin resistance and diabetes, so the jury’s still out here!). Additionally, a meta-analysis of 25 cohort studies and randomized trial follow-ups found that both high sodium and low sodium intakes were associated with increased risk of mortality, suggesting a U-shaped curve in which both too much and too little sodium can be a problem.
Want to Know ALL the Easy Steps to Nutrivore?
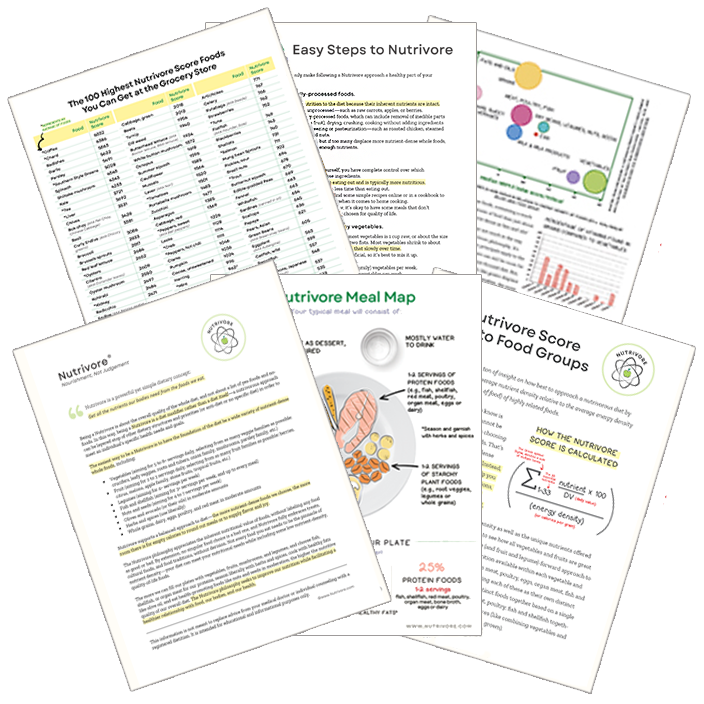
Get it Directly in Your Inbox!
The Nutrivore Newsletter is a weekly email that delivers bite-size fun facts, practical tips, recipes and resources. Sign up now and get 5 free guides directly to your inbox:
- Easy Steps to Nutrivore 4-page guide
- Nutrivore Foundational Foods 6-page guide
- Nutrivore Score Guide to Food Groups 3-page guide
- Nutrivore Meal Map
- Top 100 Nutrivore Score Foods
Health Effects of Sodium Deficiency
Although sodium deficiency rarely happens from inadequate intake (since the body readily adjusts sodium and water excretion or retention as needed, and daily sodium intake is high for most people), a condition called hyponatremia occurs when sodium levels drop too low in the blood (beneath 135 mEq/L). When this happens, it causes brain cells to swell and produces symptoms such as confusion, lethargy, nausea, vomiting, and altered personality. In severe cases (blood sodium under 115 mEq/L), hyponatremia can lead to muscle twitching, spasms, seizures, stupor, coma, and even death. Ongoing hyponatremia, even when mild, has also been associated with an increase risk of falls, bone loss, fractures, stroke, coronary heart disease events, heart disease mortality, and all-cause mortality.
Hyponatremia is most common in people with kidney disease, heart disease, liver disease, or hypertension, as well as in older adults in general. It can also occur due to extended vomiting or diarrhea (which causes the loss of sodium and other electrolytes), or the use of certain medications (such as thiazide diuretics, opiate derivatives, SSRIs, tricyclic antidepressants, and phenothiazines).
Hyponatremia is also known to occur as a result of fluid overload during endurance exercise—a condition known as exercise-associated hyponatremia. This is most common within 24 hours of sustained endurance or ultra-endurance exercise events (such as marathons, hiker treks, open-water swimming events, triathlons, and mountain bike races). In these situations, hyponatremia can occur due to excessive water intake, very low or very high environmental temperatures, or impaired water excretion through the urine (due to persistent vasopressin secretion). Pre-exercise over-hydration and the use of nonsteroidal anti-inflammatory drugs can increase the risk of exercise-associated hyponatremia.
Even when not acute, hyponatremia may cause long-term harm. In dozens of observational studies of people with a variety of medical conditions (including liver cirrhosis, cardiovascular disease, and pulmonary infections), chronic low blood sodium levels have been associated with a nearly three-times-higher risk of mortality, compared to when blood sodium levels are normal. In addition, a meta-analysis of fifteen studies found that restoring low blood sodium levels back to normal was associated with a 43% reduction in mortality risk, especially among older people and those with the lowest initial blood sodium levels.
How Much Sodium Do We Need?
In general, most people don’t need to worry about dietary sodium deficiency; recommendations are far more often to cut back! The current adequate intake level is set at 1.5 g (1500 mg of sodium) per day for adolescents and adults, which is the equivalent of 3.8 g (3800 mg) daily of table salt. Likewise, most health organizations recommend keeping sodium intake under 2.3 g per day—although given that both high and low sodium intakes have been linked with adverse effects, it may be advisable to avoid low-sodium diets unless a specific health situation warrants it, and instead focus on consuming a varied diet that contains enough potassium and calcium.
Nutrient Daily Values
Nutrition requirements and recommended nutrient intake for infants, children, adolescents, adults, mature adults, and pregnant and lactating individuals.

Merch and Household Goods
Check out our collection of practical and nerdtastic T-shirts, totes, and more!
Citations
Expand to see all scientific references for this article.
Adler AJ, Taylor F, Martin N, Gottlieb S, Taylor RS, Ebrahim S. Reduced dietary salt for the prevention of cardiovascular disease. Cochrane Database Syst Rev. 2014 Dec 18;2014(12):CD009217. doi: 10.1002/14651858.CD009217.pub3.
Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, Lin PH, Karanja N. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997 Apr 17;336(16):1117-24. doi: 10.1056/NEJM199704173361601.
Ares GR, Ortiz PA. Direct renal effects of a fructose-enriched diet: interaction with high salt intake. Am J Physiol Regul Integr Comp Physiol. 2015 Nov 1;309(9):R1078-81. doi: 10.1152/ajpregu.00156.2015.
Armando I, Villar VA, Jose PA. Genomics and Pharmacogenomics of Salt-sensitive Hypertension. Curr Hypertens Rev. 2015;11(1):49-56.
Barba G, Galletti F, Cappuccio FP, Siani A, Venezia A, Versiero M, Della Valle E, Sorrentino P, Tarantino G, Farinaro E, Strazzullo P. Incidence of hypertension in individuals with different blood pressure salt-sensitivity: results of a 15-year follow-up study. J Hypertens. 2007 Jul;25(7):1465-71. doi: 10.1097/HJH.0b013e3281139ebd.
Bedford JL, Barr SI. Higher urinary sodium, a proxy for intake, is associated with increased calcium excretion and lower hip bone density in healthy young women with lower calcium intakes. Nutrients. 2011 Nov;3(11):951-61. doi: 10.3390/nu3110951.
Bergin IL, Sheppard BJ, Fox JG. Helicobacter pylori infection and high dietary salt independently induce atrophic gastritis and intestinal metaplasia in commercially available outbred Mongolian gerbils. Dig Dis Sci. 2003 Mar;48(3):475-85. doi: 10.1023/a:1022524313355.
Blanch N, Clifton PM, Petersen KS, Keogh JB. Effect of sodium and potassium supplementation on vascular and endothelial function: a randomized controlled trial. Am J Clin Nutr. 2015 May;101(5):939-46. doi: 10.3945/ajcn.114.105197.
Boero R, Pignataro A, Quarello F. Salt intake and kidney disease. J Nephrol. 2002 May-Jun;15(3):225-9.
Borghi L, Schianchi T, Meschi T, Guerra A, Allegri F, Maggiore U, Novarini A. Comparison of two diets for the prevention of recurrent stones in idiopathic hypercalciuria. N Engl J Med. 2002 Jan 10;346(2):77-84. doi: 10.1056/NEJMoa010369.
Brown MK, Song J, MacGregor GA, Tan M, He FJ. Better Late Than Never: The FDA’s Sodium Reduction Targets. Am J Public Health. 2022 Feb;112(2):191-193. doi: 10.2105/AJPH.2021.306627.
Burger H, Grobbee DE, Drüeke T. Osteoporosis and salt intake. Nutr Metab Cardiovasc Dis. 2000 Feb;10(1):46-53.
Cappuccio FP, MacGregor GA. Does potassium supplementation lower blood pressure? A meta-analysis of published trials. J Hypertens. 1991 May;9(5):465-73. doi: 10.1097/00004872-199105000-00011.
Centers for Disease Control and Prevention (CDC). CDC grand rounds: dietary sodium reduction – time for choice. MMWR Morb Mortal Wkly Rep. 2012 Feb 10;61(5):89-91.
Cohen AJ, Roe FJ. Review of risk factors for osteoporosis with particular reference to a possible aetiological role of dietary salt. Food Chem Toxicol. 2000 Feb-Mar;38(2-3):237-53. doi: 10.1016/s0278-6915(99)00145-3.
Corona G, Giuliani C, Parenti G, Norello D, Verbalis JG, Forti G, Maggi M, Peri A. Moderate hyponatremia is associated with increased risk of mortality: evidence from a meta-analysis. PLoS One. 2013 Dec 18;8(12):e80451. doi: 10.1371/journal.pone.0080451.
Corona G, Giuliani C, Verbalis JG, Forti G, Maggi M, Peri A. Hyponatremia improvement is associated with a reduced risk of mortality: evidence from a meta-analysis. PLoS One. 2015 Apr 23;10(4):e0124105. doi: 10.1371/journal.pone.0124105.
D’Elia L, Rossi G, Ippolito R, Cappuccio FP, Strazzullo P. Habitual salt intake and risk of gastric cancer: a meta-analysis of prospective studies. Clin Nutr. 2012 Aug;31(4):489-98. doi: 10.1016/j.clnu.2012.01.003.
Devine A, Criddle RA, Dick IM, Kerr DA, Prince RL. A longitudinal study of the effect of sodium and calcium intakes on regional bone density in postmenopausal women. Am J Clin Nutr. 1995 Oct;62(4):740-5. doi: 10.1093/ajcn/62.4.740.
Dickinson KM, Clifton PM, Keogh JB. Endothelial function is impaired after a high-salt meal in healthy subjects. Am J Clin Nutr. 2011 Mar;93(3):500-5. doi: 10.3945/ajcn.110.006155.
DuPont JJ, Greaney JL, Wenner MM, Lennon-Edwards SL, Sanders PW, Farquhar WB, Edwards DG. High dietary sodium intake impairs endothelium-dependent dilation in healthy salt-resistant humans. J Hypertens. 2013 Mar;31(3):530-6. doi: 10.1097/HJH.0b013e32835c6ca8.
EFSA Panel on Nutrition, Novel Foods and Food Allergens (NDA), Turck D, Castenmiller J, de Henauw S, Hirsch-Ernst KI, Kearney J, Knutsen HK, Maciuk A, Mangelsdorf I, McArdle HJ, Pelaez C, Pentieva K, Siani A, Thies F, Tsabouri S, Vinceti M, Aggett P, Fairweather-Tait S, Martin A, Przyrembel H, de Sesmaisons-Lecarré A, Naska A. Dietary reference values for chloride. EFSA J. 2019 Sep 4;17(9):e05779. doi: 10.2903/j.efsa.2019.5779.
Ekinci EI, Clarke S, Thomas MC, Moran JL, Cheong K, MacIsaac RJ, Jerums G. Dietary salt intake and mortality in patients with type 2 diabetes. Diabetes Care. 2011 Mar;34(3):703-9. doi: 10.2337/dc10-1723.
Elfassy T, Yi S, Eisenhower D, Lederer A, Curtis CJ. Use of sodium information on the nutrition facts label in New York City adults with hypertension. J Acad Nutr Diet. 2015 Feb;115(2):278-283. doi: 10.1016/j.jand.2014.08.027.
Franco V, Oparil S. Salt sensitivity, a determinant of blood pressure, cardiovascular disease and survival. J Am Coll Nutr. 2006 Jun;25(3 Suppl):247S-255S. doi: 10.1080/07315724.2006.10719574.
Gaddy JA, Radin JN, Loh JT, Zhang F, Washington MK, Peek RM Jr, Algood HM, Cover TL. High dietary salt intake exacerbates Helicobacter pylori-induced gastric carcinogenesis. Infect Immun. 2013 Jun;81(6):2258-67. doi: 10.1128/IAI.01271-12.
Gancz H, Jones KR, Merrell DS. Sodium chloride affects Helicobacter pylori growth and gene expression. J Bacteriol. 2008 Jun;190(11):4100-5. doi: 10.1128/JB.01728-07.
Garg R, Williams GH, Hurwitz S, Brown NJ, Hopkins PN, Adler GK. Low-salt diet increases insulin resistance in healthy subjects. Metabolism. 2011 Jul;60(7):965-8. doi: 10.1016/j.metabol.2010.09.005.
Gijsbers L, Dower JI, Schalkwijk CG, Kusters YH, Bakker SJ, Hollman PC, Geleijnse JM. Effects of sodium and potassium supplementation on endothelial function: a fully controlled dietary intervention study. Br J Nutr. 2015 Nov 14;114(9):1419-26. doi: 10.1017/S0007114515002986.
Giuliani C, Peri A. Effects of Hyponatremia on the Brain. J Clin Med. 2014 Oct 28;3(4):1163-77. doi: 10.3390/jcm3041163.
Golledge J, Moxon JV, Jones RE, Hankey GJ, Yeap BB, Flicker L, Norman PE. Reported Amount of Salt Added to Food Is Associated with Increased All-Cause and Cancer-Related Mortality in Older Men in a Prospective Cohort Study. J Nutr Health Aging. 2015 Oct;19(8):805-11. doi: 10.1007/s12603-015-0483-2.
Graudal N, Hubeck-Graudal T, Jürgens G, McCarron DA. The significance of duration and amount of sodium reduction intervention in normotensive and hypertensive individuals: a meta-analysis. Adv Nutr. 2015 Mar 13;6(2):169-77. doi: 10.3945/an.114.007708.
Graudal N, Jürgens G, Baslund B, Alderman MH. Compared with usual sodium intake, low- and excessive-sodium diets are associated with increased mortality: a meta-analysis. Am J Hypertens. 2014 Sep;27(9):1129-37. doi: 10.1093/ajh/hpu028.
Graudal NA, Hubeck-Graudal T, Jurgens G. Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane Database Syst Rev. 2020 Dec 12;12(12):CD004022. doi: 10.1002/14651858.CD004022.pub5.
Greenland P. Beating high blood pressure with low-sodium DASH. N Engl J Med. 2001 Jan 4;344(1):53-5. doi: 10.1056/NEJM200101043440109.
He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ. 2013 Apr 3;346:f1325. doi: 10.1136/bmj.f1325.
Holm JP, Amar AOS, Hyldstrup L, Jensen JEB. Hyponatremia, a risk factor for osteoporosis and fractures in women. Osteoporos Int. 2016 Mar;27(3):989-1001. doi: 10.1007/s00198-015-3370-0.
Jansson B. Geographic cancer risk and intracellular potassium/sodium ratios. Cancer Detect Prev. 1986;9(3-4):171-94.
Kato S, Tsukamoto T, Mizoshita T, Tanaka H, Kumagai T, Ota H, Katsuyama T, Asaka M, Tatematsu M. High salt diets dose-dependently promote gastric chemical carcinogenesis in Helicobacter pylori-infected Mongolian gerbils associated with a shift in mucin production from glandular to surface mucous cells. Int J Cancer. 2006 Oct 1;119(7):1558-66. doi: 10.1002/ijc.21810.
Kleinewietfeld M, Manzel A, Titze J, Kvakan H, Yosef N, Linker RA, Muller DN, Hafler DA. Sodium chloride drives autoimmune disease by the induction of pathogenic TH17 cells. Nature. 2013 Apr 25;496(7446):518-22. doi: 10.1038/nature11868.
Krementsov DN, Case LK, Hickey WF, Teuscher C. Exacerbation of autoimmune neuroinflammation by dietary sodium is genetically controlled and sex specific. FASEB J. 2015 Aug;29(8):3446-57. doi: 10.1096/fj.15-272542.
Kumanyika SK, Cook NR, Cutler JA, Belden L, Brewer A, Cohen JD, Hebert PR, Lasser VI, Raines J, Raczynski J, Shepek L, Diller L, Whelton PK, Yamamoto M; Trials of Hypertension Prevention Collaborative Research Group. Sodium reduction for hypertension prevention in overweight adults: further results from the Trials of Hypertension Prevention Phase II. J Hum Hypertens. 2005 Jan;19(1):33-45. doi: 10.1038/sj.jhh.1001774.
Kurtz TW, Pravenec M, DiCarlo SE. Will Food and Drug Administration Guidance to Reduce the Salt Content of Processed Foods Reduce Salt Intake and Save Lives? Hypertension. 2022 Apr;79(4):809-812. doi: 10.1161/HYPERTENSIONAHA.121.18942.
Luft FC, Weinberger MH. Heterogeneous responses to changes in dietary salt intake: the salt-sensitivity paradigm. Am J Clin Nutr. 1997 Feb;65(2 Suppl):612S-617S. doi: 10.1093/ajcn/65.2.612S.
Maluly HDB, Arisseto-Bragotto AP, Reyes FGR. Monosodium glutamate as a tool to reduce sodium in foodstuffs: Technological and safety aspects. Food Sci Nutr. 2017 Jul 13;5(6):1039-1048. doi: 10.1002/fsn3.499.
Matthews EL, Brian MS, Ramick MG, Lennon-Edwards S, Edwards DG, Farquhar WB. High dietary sodium reduces brachial artery flow-mediated dilation in humans with salt-sensitive and salt-resistant blood pressure. J Appl Physiol (1985). 2015 Jun 15;118(12):1510-5. doi: 10.1152/japplphysiol.00023.2015.
McMahon EJ, Campbell KL, Bauer JD, Mudge DW. Altered dietary salt intake for people with chronic kidney disease. Cochrane Database Syst Rev. 2015 Feb 18;(2):CD010070. doi: 10.1002/14651858.CD010070.pub2. Update in: Cochrane Database Syst Rev. 2021 Jun 24;6:CD010070.
Mickleborough TD, Gotshall RW. Dietary salt intake as a potential modifier of airway responsiveness in bronchial asthma. J Altern Complement Med. 2004 Aug;10(4):633-42. doi: 10.1089/acm.2004.10.633.
Mozaffarian D, Fahimi S, Singh GM, Micha R, Khatibzadeh S, Engell RE, Lim S, Danaei G, Ezzati M, Powles J; Global Burden of Diseases Nutrition and Chronic Diseases Expert Group. Global sodium consumption and death from cardiovascular causes. N Engl J Med. 2014 Aug 14;371(7):624-34. doi: 10.1056/NEJMoa1304127.
Mu J, Zheng S, Lian Q, Liu F, Liu Z. Evolution of blood pressure from adolescents to youth in salt sensitivies: a 18-year follow-up study in Hanzhong children cohort. Nutr J. 2012 Sep 14;11:70. doi: 10.1186/1475-2891-11-70.
Nakajima K, Oda E, Kanda E. The association of serum sodium and chloride levels with blood pressure and estimated glomerular filtration rate. Blood Press. 2016;25(1):51-7. doi: 10.3109/08037051.2015.1090711.
National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Food and Nutrition Board; Committee to Review the Dietary Reference Intakes for Sodium and Potassium. Dietary Reference Intakes for Sodium and Potassium. Oria M, Harrison M, Stallings VA, editors. Washington (DC): National Academies Press (US); 2019 Mar 5.
Odai T, Terauchi M, Okamoto D, Hirose A, Miyasaka N. Unsalted tomato juice intake improves blood pressure and serum low-density lipoprotein cholesterol level in local Japanese residents at risk of cardiovascular disease. Food Sci Nutr. 2019 May 15;7(7):2271-2279. doi: 10.1002/fsn3.1066.
O’Donnell MJ, Yusuf S, Mente A, Gao P, Mann JF, Teo K, McQueen M, Sleight P, Sharma AM, Dans A, Probstfield J, Schmieder RE. Urinary sodium and potassium excretion and risk of cardiovascular events. JAMA. 2011 Nov 23;306(20):2229-38. doi: 10.1001/jama.2011.1729.
Oparil S. Low sodium intake–cardiovascular health benefit or risk? N Engl J Med. 2014 Aug 14;371(7):677-9. doi: 10.1056/NEJMe1407695.
Ras RT, Streppel MT, Draijer R, Zock PL. Flow-mediated dilation and cardiovascular risk prediction: a systematic review with meta-analysis. Int J Cardiol. 2013 Sep 20;168(1):344-51. doi: 10.1016/j.ijcard.2012.09.047.
Resnick LM, Gupta RK, DiFabio B, Barbagallo M, Mann S, Marion R, Laragh JH. Intracellular ionic consequences of dietary salt loading in essential hypertension. Relation to blood pressure and effects of calcium channel blockade. J Clin Invest. 1994 Sep;94(3):1269-76. doi: 10.1172/JCI117445.
Safar ME, Thuilliez C, Richard V, Benetos A. Pressure-independent contribution of sodium to large artery structure and function in hypertension. Cardiovasc Res. 2000 May;46(2):269-76. doi: 10.1016/s0008-6363(99)00426-5.
Sellmeyer DE, Schloetter M, Sebastian A. Potassium citrate prevents increased urine calcium excretion and bone resorption induced by a high sodium chloride diet. J Clin Endocrinol Metab. 2002 May;87(5):2008-12. doi: 10.1210/jcem.87.5.8470.
Snetselaar LG, de Jesus JM, DeSilva DM, Stoody EE. Dietary Guidelines for Americans, 2020-2025: Understanding the Scientific Process, Guidelines, and Key Recommendations. Nutr Today. 2021 Nov-Dec;56(6):287-295. doi: 10.1097/NT.0000000000000512.
Sundström B, Johansson I, Rantapää-Dahlqvist S. Interaction between dietary sodium and smoking increases the risk for rheumatoid arthritis: results from a nested case-control study. Rheumatology (Oxford). 2015 Mar;54(3):487-93. doi: 10.1093/rheumatology/keu330.
Tatematsu M, Takahashi M, Fukushima S, Hananouchi M, Shirai T. Effects in rats of sodium chloride on experimental gastric cancers induced by N-methyl-N-nitro-N-nitrosoguanidine or 4-nitroquinoline-1-oxide. J Natl Cancer Inst. 1975 Jul;55(1):101-6. doi: 10.1093/jnci/55.1.101.
Thomas MC, Moran J, Forsblom C, Harjutsalo V, Thorn L, Ahola A, Wadén J, Tolonen N, Saraheimo M, Gordin D, Groop PH; FinnDiane Study Group. The association between dietary sodium intake, ESRD, and all-cause mortality in patients with type 1 diabetes. Diabetes Care. 2011 Apr;34(4):861-6. doi: 10.2337/dc10-1722. Epub 2011 Feb 9.
Tsugane S. Salt, salted food intake, and risk of gastric cancer: epidemiologic evidence. Cancer Sci. 2005 Jan;96(1):1-6. doi: 10.1111/j.1349-7006.2005.00006.x.
Urso C, Brucculeri S, Caimi G. Physiopathological, Epidemiological, Clinical and Therapeutic Aspects of Exercise-Associated Hyponatremia. J Clin Med. 2014 Nov 12;3(4):1258-75. doi: 10.3390/jcm3041258.
Wannamethee SG, Shaper AG, Lennon L, Papacosta O, Whincup P. Mild hyponatremia, hypernatremia and incident cardiovascular disease and mortality in older men: A population-based cohort study. Nutr Metab Cardiovasc Dis. 2016 Jan;26(1):12-9. doi: 10.1016/j.numecd.2015.07.008.
Weinberger MH. Salt sensitivity of blood pressure in humans. Hypertension. 1996 Mar;27(3 Pt 2):481-90. doi: 10.1161/01.hyp.27.3.481.
Weir MR, Fink JC. Salt intake and progression of chronic kidney disease: an overlooked modifiable exposure? A commentary. Am J Kidney Dis. 2005 Jan;45(1):176-88. doi: 10.1053/j.ajkd.2004.08.041.
Whelton PK, Appel LJ, Espeland MA, Applegate WB, Ettinger WH Jr, Kostis JB, Kumanyika S, Lacy CR, Johnson KC, Folmar S, Cutler JA. Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in the elderly (TONE). TONE Collaborative Research Group. JAMA. 1998 Mar 18;279(11):839-46. doi: 10.1001/jama.279.11.839.
Wu C, Yosef N, Thalhamer T, Zhu C, Xiao S, Kishi Y, Regev A, Kuchroo VK. Induction of pathogenic TH17 cells by inducible salt-sensing kinase SGK1. Nature. 2013 Apr 25;496(7446):513-7. doi: 10.1038/nature11984.
Yin X, Rodgers A, Perkovic A, Huang L, Li KC, Yu J, Wu Y, Wu JHY, Marklund M, Huffman MD, Miranda JJ, Di Tanna GL, Labarthe D, Elliott P, Tian M, Neal B. Effects of salt substitutes on clinical outcomes: a systematic review and meta-analysis. Heart. 2022 Sep 26;108(20):1608-1615. doi: 10.1136/heartjnl-2022-321332.
Zaino CJ, Maheshwari AV, Goldfarb DS. Impact of mild chronic hyponatremia on falls, fractures, osteoporosis, and death. Am J Orthop (Belle Mead NJ). 2013 Nov;42(11):522-7.
Zhang WC, Zheng XJ, Du LJ, Sun JY, Shen ZX, Shi C, Sun S, Zhang Z, Chen XQ, Qin M, Liu X, Tao J, Jia L, Fan HY, Zhou B, Yu Y, Ying H, Hui L, Liu X, Yi X, Liu X, Zhang L, Duan SZ. High salt primes a specific activation state of macrophages, M(Na). Cell Res. 2015 Aug;25(8):893-910. doi: 10.1038/cr.2015.87.