Key Takeaways (expand)
- Eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) are polyunsaturated fats, collectively referred to as long-chain omega-3 fats.
- EPA and DHA aren’t technically essential, since EPA can be synthesized from alpha-linolenic acid (ALA) and then further converted to DHA. But, this conversion process is highly inefficient, so dietary sources are still valuable!
- Excess omega-6 intake can interfere with omega-3 metabolism due to competition for conversion enzymes; this makes the dietary balance of omega-3 to omega-6 fats important.
- EPA and DHA are components of the cell membrane, influencing important structural properties like membrane permeability, fluidity, and flexibility.
- EPA and DHA help form prostaglandins, thromboxanes, and leukotrienes—classes of messenger molecules variously needed for mediating inflammation, cell growth, blood clotting, kidney function, stomach acid secretion, vasoconstriction, immune responses, and pain signaling.
- Although EPA and DHA have many similar health effects, they also have some differences: DHA plays a bigger role in eye health, vision, and nervous system health (it makes up much of the brain’s fat content); EPA plays a bigger role in membrane stabilization and blood lipid modification.
- EPA and DHA can support cardiovascular health through their anti-inflammatory, anti-thrombotic (blood clotting), anti-arrhythmia, and triglyceride-lowering activity; however, findings have been mixed for whether EPA and DHA supplements impact actual cardiovascular disease outcomes and mortality.
- The inconsistent findings regarding EPA, DHA, and heart health may be due to differences in dosing, supplement form, whether the fats have oxidized, the ratio of EPA to DHA, participants’ baseline EPA and DHA status, and genetic variation.
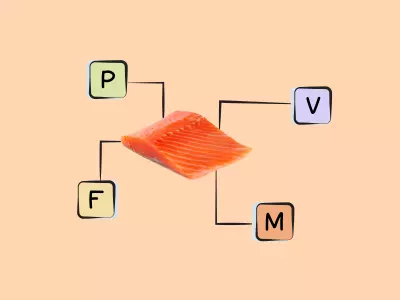
- When it comes to whole-food sources of EPA and DHA like fatty fish, the findings show a much more consistent benefit for cardiovascular health—including reduced risk of heart attack, heart failure, stroke, and heart disease mortality.
- EPA and DHA possess a number of benefits for neurological health and brain function; higher blood levels are associated with a reduced risk of depression, ADHD, bipolar disorder, autism, schizophrenia, and dementia.
- Trials of EPA and DHA supplementation have been shown to help reduce ADHD symptoms in children, cognitive decline in the elderly, and anxiety, while also showing similar effectiveness as pharmaceutical drugs for depression.
- These neurological benefits may be due to EPA and DHA preserving neuron function and cell membrane integrity in the brain, as well as reducing brain inflammation, increasing neurogenesis, enhancing cerebral blood flow, and modulating neurotransmission.
- During pregnancy, EPA and DHA can help improve gestational diabetes, reduce the risk of premature or very low birth weight delivery, and help the fetus properly develop.
- EPA and DHA supplementation during pregnancy is associated with benefits for the child after birth, including enhanced problem solving, improved hand and eye coordination, and decreased incidence of asthma, food allergies, and eczema.
- EPA and DHA can support gut health, including improving microbial diversity, lowering gut inflammation, reducing levels of harmful bacteria, and increasing levels of probiotic microbes like Bifidobacterium and Lactobacillus.
- Inadequate intake of EPA and DHA can increase the risk of cardiovascular disease, inflammatory skin conditions, obesity, mood disorders, joint pain and stiffness, and dry eyes.
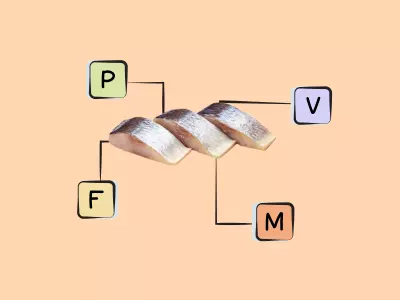
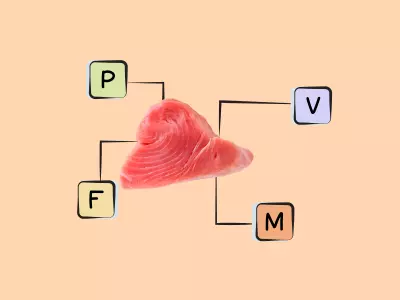
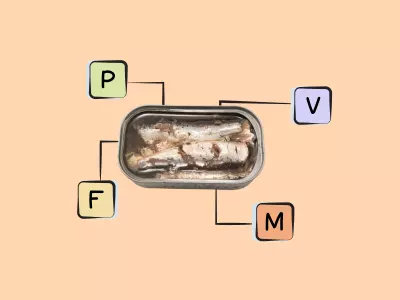
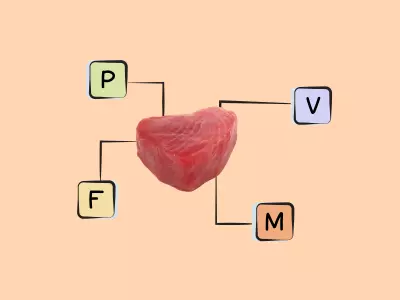
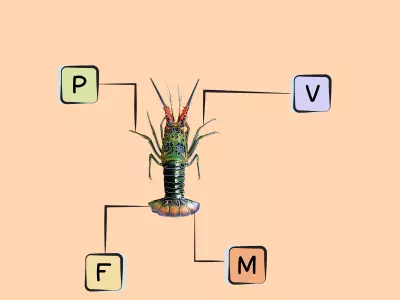
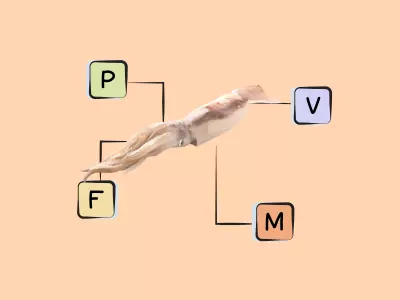
- The best sources of DHA and EPA are fish (particularly fatty cold-water fish like salmon, herring, mackerel, sardines, and menhaden), algaes, cod liver oil, and shellfish.
Table of Contents[Hide][Show]
EPA and DHA in Health and Disease+−
- EPA and DHA and Cardiovascular Disease
- EPA and DHA, Neurological Health and Mental Health
- EPA and DHA and Autoimmune Disease
- EPA and DHA and Pregnancy
- EPA and DHA and Gut Health
- EPA and DHA and Sarcopenia
- EPA and DHA and Cancer
- EPA and DHA and Chronic Fatigue Syndrome
- EPA and DHA and Celiac Disease
- EPA and DHA and Type 2 Diabetes
- EPA and DHA and Skin Health
- EPA and DHA and Hair
- EPA and DHA and Migraine
- EPA and DHA and Endometriosis
- EPA and DHA and Seizures
- EPA and DHA and Osteoarthritis
- EPA and DHA and Sleep
- EPA and DHA and Primary Sclerosing Cholangitis
- Health Effects of EPA and DHA Deficiency
- Problems From EPA and DHA Supplements
- How Much EPA and DHA Do We Need?
- Best Food Sources of EPA and DHA
- Good Food Sources of EPA and DHA
Eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), collectively referred to as long-chain omega-3 fats, have unique health properties and a fascinating history! Up through the early 1900s, dietary fat was believed to simply be a source of calories, interchangeable with carbohydrates and not required for life. But in 1929, George and Mildred Burr—a husband-and-wife research team—conducted a series of rat experiments revealing that certain fatty acids were critical to health, and their absence led to serious deficiency symptoms and even death. The Burrs subsequently coined the term “essential fatty acids,” and initially ascribed this essential nature only to the omega-6 fat linoleic acid. It took many more decades before omega-3s became recognized as essential, too! Eventually, in the 1970s, interest in omega-3 fats began skyrocketing when scientists discovered that the seafood-rich diet of the Greenland Inuit seemed to protect them from heart disease—leading to thousands of studies seeking to understand these special fats, as well as an entire industry built around selling them as supplements!
EPA and DHA are particularly important for fetal development, immune function, retinal health, inflammation, and some aspects of cardiovascular health (like triglyceride levels and blood clotting); they’re also a structural component of the cell membrane. Small amounts of them can be synthesized from a shorter-chain omega-3 fat, alpha-linolenic acid (ALA).
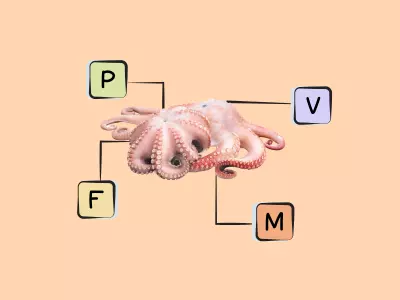
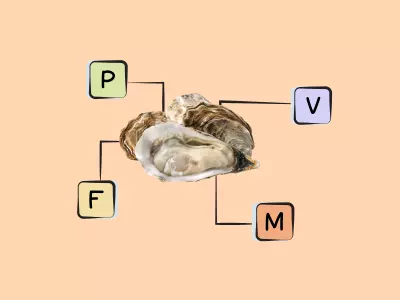
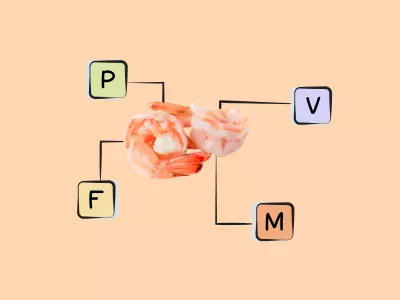
Rich sources of DHA and EPA are fish, particularly fatty cold-water fish (like salmon, herring, mackerel, sardines, and menhaden) as well as some algaes and cod liver oil. Shellfish such as mussels, crab, oysters, and squid also contain some long-chain omega-3s. There are also trace amounts in the leafy green vegetable purslane, although the type of omega-3 found in plant foods is more typically ALA!
Want to know the top 25 foods for this awesome nutrient?

The Top 25 Foods for Every Nutrient
The Top 25 Foods for Every Nutrient e-book is a well-organized, easy-to-use, grocery store-friendly guide to help you choose foods that fit your needs of 43 important nutrients while creating a balanced nutrient-dense diet.
Get two “Top 25” food lists for each nutrient, plus you’ll find RDA charts for everyone, informative visuals, fun facts, serving sizes and the 58 foods that are Nutrient Super Stars!
Buy now for instant digital access.
The Biological Roles of EPA and DHA
All omega-3 fats are characterized by a shared feature in their chemical structure: a double bond located three atoms away from their terminal methyl group. They also contain multiple other double bonds, making them “polyunsaturated” fats (in contrast to monounsaturated fats, which have only one double bond, or saturated fats, which have none). In general, omega-3 fats are used for chemical reactions within cells that produce signaling molecules involved in inflammation, blood pressure regulation, and pain perception. They’re components of the cell membrane, where they alter important structural properties like membrane permeability, fluidity, and flexibility—consequently impacting the activity of membrane receptor systems and influencing gene expression and signaling pathways. The omega-3s we consume from food alter the proportion of omega-3 fats that end up in red blood cells, cardiac tissue, immune cells, atherosclerotic plaque, and more, in turn affecting the characteristics of these cells and the function of their receptors!
Omega-3 fats compete with omega-6 fats for the same conversion enzymes, as well as for positions in cell membranes—which is why we often hear about the importance of a balanced ratio between these two families. Too much dietary omega-6 relative to omega-3 can interfere with omega-3 metabolism, and is associated with a number of chronic health conditions such as obesity, cardiovascular disease, Alzheimer’s disease, non-alcoholic fatty liver disease, inflammatory bowel disease, and rheumatoid arthritis. Historically, the human diet is estimated to have featured about a 1:1 ratio of omega-6 to omega-3 fats, whereas the modern Western diet has a ratio of 15 to 20:1 or higher (largely due to the increased consumption of omega-6 rich grains and vegetable oils, and under-consumption of omega-3 rich seafood)!
Although the most common omega-3 fats we hear about are ALA, EPA, and DHA, there are actually 11 different omega fats in total! But, these “big three” are considered most important for human health, and have been the subject of far more research than the lesser-known omega-3 fats.
Importantly, ALA is the only omega-3 fat that’s considered truly essential, because the body can’t synthesize it any way; EPA and DHA can actually be made from ALA! More specifically, when we ingest ALA, some of it undergoes a series of desaturation and elongation reactions (the addition of double bonds and carbon atoms, respectively) that results in the creation of EPA, which can then be further converted to DHA. But, this process is very inefficient, and can vary based on a person’s gender, genetics, and overall diet.
For example, women can convert more dietary ALA into EPA and DHA than men—likely due to the effects of estrogen on enzymes used for EPA and DHA synthesis. Genetic variations involving the fatty acid desaturase (FADS) genes can also influence how efficiently EPA and DHA are synthesized. Due to competition between omega-3 and omega-6 fats for the same elongase and desaturase enzymes, a high omega-6 intake (particularly linoleic acid) can reduce how much EPA and DHA are produced from ALA by as much as 40%. Saturated fatty acids, trans fats, dietary cholesterol, and even smoking can similarly disrupt the desaturation and elongation processes used to produce EPA and DHA from ALA.
So, even though the long-chain omega-3s aren’t technically essential (since they can be synthesized from another dietary fat), the extreme individual variation in conversion capacity makes it important to ingest some of these fats directly from food!
It was also once believed that DHA could be retroconverted into EPA (that is, along with EPA getting converted into DHA, DHA could get converted back into EPA), due to early studies showing that DHA supplementation led to higher circulating levels of EPA. However, more recent research suggests this isn’t really the case: consuming more DHA simply slows down the metabolism of EPA, sparing the EPA already present in the body and allowing more of it to remain in circulation. So, DHA can indeed help boost our EPA levels, but not through being converted into it!
Once in the body, EPA and DHA help form prostaglandins, thromboxanes, and leukotrienes—classes of messenger molecules that are important mediators of a variety of functions, including inflammation (hence omega-3 fats’ famous reputation for being anti-inflammatory). Prostaglandins have essential roles in a variety of systems in the human body, including being regulators of blood clotting, pain signaling, cell growth, kidney function, stomach acid secretion, and inflammation. Thromboxanes are produced by platelets and serve an essential function in blood clotting by simultaneously causing platelet aggregation and vasoconstriction. And lastly, leukotrienes are primarily synthesized by inflammatory cells and are essential mediators of inflammatory and immune responses.
Unique Activities of DHA
Although EPA and DHA do have many shared health effects, their roles aren’t identical!
For example, DHA has a specific role in eye health and vision due to being selectively incorporated into the membranes of retinal cells (especially photoreceptor cells, which convert light into signals that are then sent to the brain—ultimately allowing for vision). In fact, even when omega-3 intake is low, the retina conserves and recycles DHA in order to protect the eyes! Animal studies have shown that DHA is needed for the retina to properly develop, and if DHA is inadequate during certain periods of early life, it can result in permanent abnormalities in how the retina functions. Additional research suggests that DHA is needed for the regeneration of rhodopsin, the main photoreceptor molecule involved in vision.
DHA also plays an important role in nervous system health. In fact, it serves as a major component of neuronal plasma membranes, and makes up about 40% of the polyunsaturated fatty acid content of the brain. Along with being incorporated into postsynaptic cells (neuron cells that receive signals), DHA increases the release of the neurotransmitter acetylcholine, which plays a role in brain plasticity and memory. This fat also helps modulate the transport of glycine, taurine, and choline!
Some in vitro studies have shown that EPA and DHA can modulate ion channel conductance, in turn decreasing the excitability of muscle cells in the heart. Among the omega-3 fats, DHA is also preferentially taken up by the heart muscle, and metabolizes towards resolvins—anti-inflammatory mediator molecules that directly influence cardiac function. Due to their molecular structure, all omega-3 fats are relatively prone to oxidation: their multiple double bonds can attract electrons from nearby carbons, resulting in oxidation. This is important to keep in mind, because some studies of dietary omega-3 intake can be confounded by the way omega-3-rich foods or supplements are prepared or stored.
Nutrivore Is a Game-Changer—These 5 Free Guides Show You Why
Sign up for the free weekly Nutrivore Newsletter and get 5 high-value downloads—delivered straight to your inbox—that make healthy eating simple and sustainable.

EPA and DHA in Health and Disease
EPA and DHA can support cardiovascular health by exerting anti-inflammatory, anti-arrhythmia, anti-thrombotic, and triglyceride-lowering properties, although whole-food sources like fatty fish appear more protective of actual cardiovascular outcomes than isolated supplements. They also possess benefits for neurological health and brain function, with studies showing that supplementing with these fats can help reduce symptoms of anxiety, childhood ADHD, cognitive decline in the elderly, and depression. During pregnancy, EPA and DHA are particularly important for fetal development—offering cognitive and immune benefits that carry over into childhood. EPA and DHA can likewise support gut health by lowering gut inflammation, increasing microbial diversity, and beneficially altering the composition of the microbiota towards lower levels of harmful bacteria and higher levels of beneficial probiotic species!
EPA and DHA and Cardiovascular Disease
EPA and DHA have a popular reputation for being heart-healthy, and a great deal of research has been dedicated to this topic! In observational studies, higher omega-3 intake, greater seafood consumption, and blood levels of omega-3 have all been associated with reduced risk of cardiovascular disease, as well as improvements in cardiovascular disease risk factors. And, there are certainly mechanisms through which EPA and DHA would be expected to benefit heart health—including helping stabilize cell membranes, exhibiting anti-inflammatory and anti-thrombotic (blood clotting) activity, protecting against heart arrhythmia, and lowering triglyceride levels (one of their best-proven effects). In fact, research shows that for people with baseline high triglycerides, supplemental EPA and DHA (at doses of 4 g of omega-3 fats in total) can lower triglyceride levels by 30% or more.
But, the evidence from studies has been surprisingly inconsistent, especially when we look controlled trials rather than epidemiological research (as well as studies of EPA and DHA supplements versus whole-food sources—particularly fish!). While early omega-3 intervention trials showed promise for the primary or secondary prevention of cardiovascular disease outcomes, later research cast doubt on those initial findings. For example, in 2018, two of the largest and longest randomized controlled trials on omega-3 supplements and cardiovascular disease were published: one following more than 15,000 participants for an average of 7.4 years, and one following more than 25,000 participants for an average of 5.3 years. In both studies, there was no benefit of long-chain omega-3 supplements over placebo in preventing major cardiovascular events, like heart attack or stroke. Likewise, a meta-analysis of 19 randomized controlled trials of people with impaired glucose metabolism or diabetes (significant risk factors for cardiovascular disease) found that while omega-3 supplements were generally helpful at reducing triglycerides, there was no effect on other markers of cardiovascular health (including cholesterol levels, blood pressure, heart rate, or endothelial function), nor was there any reduction in actual cardiovascular events or mortality over time. Yet another meta-analysis of only the largest randomized omega-3 trials, each lasting at a year or more, found no significant associations between long-chain omega-3 supplements and subsequent cardiovascular events or mortality. Those findings held true even when analyzing the data by specific sub-populations, such as people with previous heart disease, high cholesterol, diabetes, or statin use.
But, some recent meta-analyses have also yielded more supportive results, adding to the confusion! For example, one assessment of omega-3 trials found that while the most common dose (1 g daily) had no association with cardiovascular disease outcomes, higher doses (2 – 4 g daily) appeared potentially protective against cardiac death. Additionally, a 2022 meta-analysis of randomized trials did find significant associations between long-chain omega-3 supplement use and reduced risk of major adverse cardiovascular events, cardiovascular death, and heart attack (although there was no apparent effect on stroke or all-cause mortality).
These contradictory findings could be due to a number of factors. For one, omega-3 studies differ in the EPA and DHA preparations they use: some trials use ethyl esters, some use free fatty acids, and some use fish oil. It’s possible that the differences in structures of the omega-3 fats given to participants could affect health outcomes, especially if more oxidation-prone preparations are used (given that oxidized lipids are harmful to cardiovascular health!). Likewise, it’s possible that the dose typically used in studies (1 g of omega-3 fats daily) is too low to produce benefits, or that the particular ratio of EPA to DHA used in the supplements influences their effects on health.
Patients’ baseline EPA and DHA status may also impact how they respond to supplementation. Some research shows that omega-3 supplements are most effective at boosting the cardiovascular health of people initially consuming very little omega-3s, suggesting that populations with generally higher seafood consumption might benefit less from additional EPA and DHA. Genetic variations, too, could play a role in how omega-3 supplements affect health; for example, carriers of the APOE4 phenotype appear less able to utilize dietary DHA, and may therefore obtain fewer benefits from omega-3 supplements (or, alternatively, need much higher doses to see any effects!).
Additionally, some research has suggested that isolated EPA supplementation is more effective than EPA and DHA combined at reducing cardiovascular mortality, heart attacks, and other cardiovascular events—especially among people with a history of heart disease. Although we don’t have clear mechanisms for why this would be the case, it’s possible that in supplement form, DHA could offset some of the cardio-protective effects unique to EPA—such as its greater impact on membrane stabilization (in contrast to DHA increasing membrane fluidity), its greater ability to limit oxidized LDL levels in the blood, and its ability to lower triglycerides without raising LDL (whereas some studies of DHA have shown it can modestly increase LDL levels). However, some of these EPA-only studies also showed a higher risk of atrial fibrillation among participants, and some follow-ups to the early trials ended up finding no reduced risk over time among the EPA group versus placebo. So, much more research would be needed to replicate the initial positive findings of these studies before EPA monotherapy could be considered safe and effective.
It’s also worth noting that not all omega-3 trials have been equal in quality! In fact, a Cochrane review of 79 randomized controlled trials—the most extensive systematic assessment published on this topic—concluded that on the whole, the studies that did show a heart-protective effect of EPA and DHA supplements were lower quality and at high risk of bias, making their findings less reliable. When analyzing only the highest-quality evidence, the heart-protective effect of these supplements remained null.
So, despite the considerable number of trials that have been conducted on EPA and DHA supplements, there’s still no definitive answer about whether they can benefit cardiovascular health, for which populations, and at what doses. Currently, there isn’t enough evidence to suggest they can significantly and consistently reduce cardiovascular events or mortality.
However, the evidence landscape changes when we look at whole-food sources of EPA and DHA! When it comes to seafood consumption rather than isolated omega-3 supplements, studies have generally been far more supportive of a cardiovascular benefit. In one meta-analysis of prospective studies, people with the highest versus lowest fish intake had a 27% reduced risk of heart attack, 20% reduced risk of heart failure, and 14% reduced risk of stroke. Another meta-analysis found that eating fish five or more times per week was associated with a 38% reduction in heart disease mortality, compared to eating fish less than once per month; likewise, every 20 g per day increase in fish consumption was associated with a 7% drop in heart disease deaths. Additional meta-analyses assessing studies by type of fish have determined that fatty fish, but not lean fish, are associated with these beneficial outcomes—indicating that the omega-3 component of seafood is what drives these heart-protective trends!
Similarly, intervention trials have been fairly consistent in showing support for omega-3-rich seafood and cardiovascular health. A meta-analysis of 14 intervention studies found that oily fish intake was associated with a significant drop in triglycerides and a significant increase in HDL cholesterol—two important biomarkers of cardiovascular risk.
However, even here, there are some caveats. In general, the cardiovascular benefits of seafood seem to depend on the type of fish being eaten (fatty or lean), cooking method (such as broiling, baking, or frying), whether environmental contaminants or heavy metals are present, and how habitually the fish is consumed. One large systematic review concluded that while non-fried fish consumption was associated with improved cardiovascular disease outcomes, fried fish was actually associated with higher risk of heart attack and other cardiovascular events. And, because whole fish contains more micronutrients than fish oil or isolated EPA and DHA supplements, other nutritional components of fish may work individually or synergistically with omega-3 fats to support cardiovascular health from multiple fronts. In other words, this is another case where nutrients from whole-food, healthfully prepared sources are likely the most health promoting.
EPA and DHA, Neurological Health and Mental Health
EPA and DHA have also been studied for their role in neurological health and brain function. In general, low omega-3 levels in the blood have been associated with a number of mood disorders and neurological conditions, including depression, bipolar disorder, ADHD, autism spectrum disorder, dementia, and schizophrenia. Likewise, evidence from additional observational and clinical research supports the idea that on the whole, these fats are a major boon for brain health and mental wellness.
Where depression is concerned, a number of observational studies have shown that higher dietary omega-3 intake is associated with lower incidence of major depressive disorder, bipolar depression, and prenatal depression. Likewise, randomized controlled trials have found that EPA and DHA (typically in the form of fish oil) may benefit patients with major depression in a way that’s comparable to leading pharmaceutical drugs—particularly fluoxetine, also known as Prozac! A meta-analysis of 26 studies found that pure EPA and EPA-dominant supplements (containing at least 60% EPA) produced major improvements in depression symptoms when doses contained at least 1 g of EPA per day. However, pure DHA and DHA-dominant supplements had no significant effect, and the evidence is less clear even for EPA when it comes to patients with minor (versus major) depression.
EPA and DHA have also shown potential for reducing the progression to psychotic disorder among people at high risk (in particular, younger individuals with sub-threshold psychotic states), reducing ADHD symptoms in children (particularly in children with low baseline omega-3 status), decreasing symptoms of anxiety (mostly at intakes of 2 g daily or more), possibly improving working memory and processing accuracy in healthy adults, and reducing the rate of cognitive decline in the elderly (at doses of 900 mg of DHA daily). A 2021 meta-analysis of 20 randomized controlled trials found that among patients with severe schizophrenia, supplementation with over 1 g of EPA daily led to significant symptom improvements.
Along with successful supplement trials, a pooled analysis of five elderly cohort studies found that eating four or more servings of fish per week (compared to less than one weekly serving) was associated with a significantly slower decline in global cognition and memory; likewise, a meta-analysis found that each additional serving of fish per week was associated with a 5% reduction in dementia risk and a 7% reduction in Alzheimer’s risk. And, EPA and DHA may support the neurological health of children: a randomized trial of healthy 8- and 9-year-old children found that the addition of 300 g of oily fish per week led to significant improvements in cognitive function (particularly cognitive flexibility and attention) while also reducing social and emotional behavioral issues.
Although researchers are still studying the exact mechanisms behind these findings, a number of possibilities exist. For one, because omega-3 fats (especially DHA) serve as a component of the phospholipid membrane of neurons, they may benefit cognition by preserving neuron function and cell membrane integrity in the brain. Likewise, the anti-inflammatory effects of EPA and DHA would be expected to reduce neuroinflammation, which itself has been implicated in mood disorders and other neurological conditions. These fats have also been shown to increase neurogenesis (the formation of new neurons), enhance cerebral blood flow, reduce amyloid aggregation, and play roles in neurotransmission (the transfer of information between neurons via chemical signaling)—all of which would be expected to benefit the brain!

Stressed? CBD May Help
- Supports sleep, helps manage stress, reduces inflammation, reduces pain
- USDA Organic, 3rd-party tested, full-spectrum hemp extract
- Available in lemon, cinnamon, mint and unflavored, all with no harsh hemp aftertaste
- Talk to your doctor about whether CBD is right for you, and how much to take
EPA and DHA and Autoimmune Disease
EPA and DHA also appear beneficial for people with systemic lupus erythematosus, an autoimmune disease involving the central nervous system. A variety of randomized controlled trials have shown that omega-3 supplements can significantly reduce disease activity—sometimes by up to 50%! These fats appear to exert a therapeutic effect for lupus by altering the body’s cytokine network, and have been most effective at relatively lower doses (160 mg of EPA and 140 mg of DHA).
People with another autoimmune condition, rheumatoid arthritis, may similarly benefit from increased EPA and DHA intake: a number of trials have shown that long-chain omega-3 supplementation can reduce pain associated with the disease, especially at intakes of 3 to 6 g daily.
EPA and DHA and Pregnancy
EPA and DHA many also offer some unique benefits during pregnancy, for mother and baby alike! For example, EPA and DHA supplementation have also been shown to improve insulin levels and inflammatory markers in women with gestational diabetes. Likewise, studies have shown that supplementing with DHA while pregnant can reduce the risk of premature or very low birth weight delivery. One dose-response analysis found that DHA supplementation of up to 600 mg daily during led to a continuous reduction in premature birth risk and very low birth weight—meaning that the higher the DHA supplementation, the greater the protective effect. These fats may help extend gestation and prevent preterm delivery by decreasing the production of certain prostaglandins, thereby lowering uterus inflammation (which has been implicated in premature labor).
And, these long-chain omega-3s are important for proper development of the fetus—including neuronal, retinal, and immune function. A variety of studies have shown that the use of omega-3 supplements during pregnancy, and/or maternal omega-3 intake in general, is associated with enhanced infant problem solving, improved hand and eye coordination during toddler years, and decreased incidence of asthma, food allergies, and eczema in children. Consuming adequate DHA, in particular, may be important during pregnancy due to the rapid accumulation of DHA in the fetus during the third trimester—especially fetal retinal and brain tissue.
EPA and DHA and Gut Health
Long-chain omega-3 fats appear incredibly supportive for gut health. In human studies, omega-3 supplementation leads to lower levels of potentially harmful bacteria and higher levels of the famous probiotics Bifidobacterium and Lactobacillus. Likewise, higher omega-3 levels in the body (reflecting higher consumption) have been linked to more microbial diversity in the gut, as well as a greater abundance of short-chain fatty acid-producing bacteria belonging to the Lachnospiraceae family. Omega-3 fats also appear capable of reversing the dysbiosis associated with irritable bowel syndrome, and their anti-inflammatory effects can benefit other disorders involving inflammation of the gut. And, while these findings would need to be confirmed in humans, rodent studies suggest that omega-3 supplementation may alter the composition of the gut microbiota in ways that reduce endotoxin production, gut permeability, inflammation, and metabolic endotoxemia—all of which influence disease risk.
Not surprisingly, EPA and DHA may also specifically benefit the inflammatory bowel diseases Crohn’s disease and ulcerative colitis. A 2014 study of over 170,000 women found that higher intakes of intake of long-chain omega-3 fats was associated with a trend towards lower risk of ulcerative colitis. Another 2014 study found inverse associations between DHA intake and the risk of developing Crohn’s disease, with participants in the highest versus lowest quintile of intake having a 46% lower risk. A 2005 randomized placebo-controlled controlled trial found that the addition of long-chain omega-3 fats (400 mg daily of EPA and 200 mg daily of DHA) to standard medication significantly reduced the number of disease relapses, helping patients remain in remission!
EPA and DHA and Sarcopenia
EPA and DHA may be useful in protecting against sarcopenia—a condition of age-related loss of muscle mass and strength. A 2019 study of 277 older adults found that sarcopenia was more prevalent among participants with low serum EPA levels. Similarly, lower blood levels of EPA were associated with lower muscle parameter values.
Controlled trials have also helped confirm a cause-and-effect relationship here! For example, a 2015 placebo-controlled trial of older women found that 12 weeks of consuming 3 g of EPA and DHA daily led to a number of favorable changes, including a 4% increase in lean mass and a 7% increase in functional capacity. And, a 2022 controlled trial of 200 older adults found that compared to placebo, six months of fish oil supplementation (1.34 g EPA and 1.07 DHA) led to significant improvements in muscle mass and strength, including increases in thigh circumference, total skeletal muscle mass, appendicular skeletal muscle mass, muscle strength, hand grip strength, and other measures of physical performance.
In general, the evidence points to consumption of at least 2 g of EPA and DHA daily for protecting against sarcopenia, with the muscle- and strength-preserving effects being due to reducing inflammation, decreasing intracellular protein breakdown, improving mitochondrial function, enhancing amino acid transport, and modulating of neuromuscular junction activity!
EPA and DHA and Cancer
Although research here has sometimes been conflicting, studies suggest a protective effect of EPA and/or DHA on certain types of cancer.
A 2013 case-control study found that while total omega-3 fat intake wasn’t associated with the risk of endometrial cancer, EPA and DHA both appeared protective. Specifically, participants in the highest versus lowest quartile of EPA intake had a 43% lower risk of endometrial cancer, while those in the highest quartile of DHA intake had a 36% lower risk! However, some other studies have found the relationship between these fatty acids and endometrial cancer to be dependent on individual factors like body weight, with the protective effect being most pronounced among normal-weight women. Some research even found an association between higher EPA and DHA intake and increased risk of endometrial cancer among overweight and obese women. Clearly, more research is needed on this topic!
Some studies also suggest a protective effect of EPA and DHA on colorectal cancer. A 2023 meta-analysis, encompassing 54 observational studies and four Mendelian Randomization studies, found that high (versus low) intake of EPA and DHA was associated with a significant 10 to 12% reduction in colorectal cancer risk. DHA was also associated with a 13% lower risk of rectal cancer, specifically.
A 2022 analysis of European Prospective Investigation into Cancer and Nutrition (EPIC) data also showed that colorectal cancer incidence decreased with increasing red blood cell concentrations of EPA. Those with higher versus lower concentrations had a 25% reduction in risk.
However, clinical trials of DHA and EPA intake have had less consistent findings. A 2020 randomized controlled trial found that supplementation with 1 g of marine omega-3 fats daily had no significant impact on the risk of colorectal cancer or serrated polyps (a colorectal tumor precursor) over the course of follow up (an average of 5.3 years). However, a subgroup analysis found that among participants with low baseline blood levels of omega-3s, supplementation was associated with a 24% lower risk.
Other research has also suggested the effects of EPA and DHA on colorectal cancer risk could vary based on baseline omega-3 fat levels, as well as other factors like ethnicity, baseline levels of inflammation, tumor characteristics, and interaction with the gut microbiota. More research is needed!
A 2020 meta-analysis of 25 observational studies, encompassing over 1.2 million participants, found that EPA and DHA were also protective against digestive system cancers—including pharyngeal cancer, esophageal cancer, and oral cavity cancer. In this analysis, higher intakes of EPA or DHA were each associated with a 21% lower risk!
EPA and DHA have also been studied in relationship to breast cancer, with promising findings! A 2023 systematic review concluded that among breast cancer patients, EPA and DHA consumption significantly improves disease progression time and overall survival. What’s more, these fats appear to help reduce surgical site healing complications, infection rates, perceived stress, depression, sleep disturbances, pain, fatigue, and joint stiffness among patients. Observational research has also found that high intakes of EPA and DHA relative to omega-6 fats tends to correlate with lower breast cancer risk.
Lastly, EPA and DHA may have some benefits for skin cancer. A 2017 study of over 20,000 women found that over the course of 4.5 years of follow-up, those in the highest versus lowest tertiles of EPA and DHA intake had an 80% lower risk of developing malignant melanoma. And, a 2021 study found that among organ transplant recipients (who have over a 100-fold greater risk of developing skin cancer compared to the general population), those with higher intakes of long-chain omega-3 fats had a substantially lower risk of developing squamous cell carcinoma.
EPA and DHA and Chronic Fatigue Syndrome
Low levels of EPA and DHA have been associated with chronic fatigue syndrome. A 2018 trial of chronic fatigue patients, for example, found that a whopping 92.6% of the studied patients had a low mean omega-3 index.
Likewise, a study from 2005 found that chronic fatigue patients had significantly lower ratios of EPA to arachidonic acid than healthy controls. There was also an inverse relationship between the patients’ overall omega-3/omega-6 ratio and their disease severity and symptoms, including aches and pains, fatigue, and failing memory. What’s more, a lower omega-3/omega-6 ratio among chronic fatigue patients was associated with defects in early T cell activation, suggesting that decreased availability of omega-3 fats (including EPA) could play a role in the development of chronic fatigue syndrome and its related immune abnormalities.
Although evidence from clinical trials is limited, several case studies found significant improvements in chronic fatigue symptoms from eight to 12 weeks of EPA supplementation. More controlled research in humans is needed!
EPA and DHA and Celiac Disease
Mechanistic studies have shown that DHA can suppress the intestinal epithelial cell inflammation induced by gliadin exposure. However, human trials are still needed!
EPA and DHA and Type 2 Diabetes
A variety of studies, ranging from animal models to observational studies to clinical trials, have suggested a promising role of EPA and/or DHA for diabetes. A 2013 randomized controlled trial found that feeding elderly type 2 diabetic patients with an EPA- and DHA-enriched diet led to significant declines in fasting plasma glucose and HbA1c, suggesting improved insulin sensitivity. Another randomized controlled trial from 2013 found that after three months of EPA supplementation (2 g daily), fasting plasma glucose, HbA1c, homeostasis model assessment of insulin resistance (HOMA-IR), and serum insulin levels all significantly decreased among overweight type 2 diabetics! A 2023 review also found that a high dietary ratio of dietary EPA to arachidonic acid (AA) tends to be associated with better glycemic control and reduced inflammation.
However, not all research has been consistent on this topic, with some studies showing no appreciable effect of EPA and DHA supplementation on diabetes risk or management. A 2015 meta-analysis of randomized controlled trials found that the EPA/DHA ratio may be impacting the results of studies: trials with a higher ratio of EPA to DHA tended to have stronger beneficial effects on on glucose control (as measured by plasma insulin and HbAc1).
Additionally, EPA and DHA may help combat some complications of diabetes, including diabetic neuropathy (diabetes-induced nerve damage) and diabetic nephropathy (diabetes-induced deterioration of kidney function). A 2019 trial of type 2 diabetics found that after three months of daily supplementation with fish oil (containing 1000 mg DHA and 200 mg EPA), participants reported significant improvements in neuropathic pain symptoms. An earlier trial from 1996 similarly found that among type 2 diabetics, EPA supplementation (1800 mg per day for 48 weeks) had significant benefits for both diabetic neuropathy and nephropathy symptoms. Studies have also found a neuroprotective effect of DHA in experimental models of diabetes!
EPA and DHA and Skin Health
Long-chain omega-3 fats could benefit skin health, including protecting against visible signs of aging and benefiting some specific skin conditions. A 2020 review of 38 studies found that supplementation with these fats may help treat psoriasis, atopic dermatitis, acne, and skin ulcers! Although evidence is more limited, some studies suggest benefits for rosacea as well.
A 2014 randomized controlled trial found that among acne patients, a combination of gamma-linolenic acid plus 2000 mg of DHA and EPA, taken daily for 10 weeks, led to significant improvements in inflammatory and non-inflammatory acne lesions. Patients’ subjective assessments of their condition also improved.
EPA and DHA and Hair
Although research is limited in humans, some studies suggest that long-chain omega-3 fats could benefit hair growth. A 2015 randomized controlled trial of women found that six months of taking a supplement containing omega-3 fats (along with omega-6 fats and antioxidants) led to significant reductions in hair loss and improvements in hair density. Of course, it’s hard to say which component(s) of the supplement drove these effects. Experimental studies have also found a beneficial effect of DHA on hair growth by promoting anagen-activating pathways. More research in humans is needed!
EPA and DHA and Migraine
Long-chain omega-3 fats could have therapeutic potential for migraine headaches! A 2018 cross-sectional study found that in a nationally representative sample of over 12,000 adults, higher dietary intakes of EPA and DHA were associated with lower headache prevalence. A 2018 systematic review and meta-analysis of randomized controlled trials likewise found that omega-3 supplementation leads to a significant reduction (approximately 3.44 hours) in migraine duration.
EPA and DHA and Endometriosis
EPA and DHA appear protective of endometriosis. A 2012 study found that the blood ratio of EPA to arachidonic acid correlated with the severity of patients’ endometriosis, and a 2015 study found that compared to women with low serum EPA levels, women with high EPA levels were a whopping 82% less likely to have endometriosis! A 2010 prospective study had similar findings for dietary consumption, showing that participants in the top fifth of long-chain omega-3 fatty acid intake were 22% less likely to be diagnosed with endometriosis, compared to participants with the lowest intake.
Intervention trials suggest EPA and DHA in the form of fish oil could help reduce pain among young women with endometriosis. And, animal experiments have also shown that long-chain omega-3 fats influence immune, angiogenic (blood vessel forming), and proliferative (growing and increasing) factors involved in the early stages of endometriosis.
EPA and DHA and Seizures
A number of studies have found long-chain omega-3 fats to be beneficial for seizure disorders, such as epilepsy. A 2018 randomized, double-blind, placebo-controlled trial of patients with drug-resistant epilepsy found that both EPA and DHA supplementation were effective for reducing seizure frequency. Compared to placebo, one year of daily supplementation with EPA reduced seizure frequency by 42%, while a year of daily supplementation with DHA reduced it by 39%!
A 2015 clinical trial using fish oil had similar findings, with low-dose fish oil supplementation (a combined total of 1080 mg EPA plus DHA) leading to a 33% reduction in seizure frequency—though interestingly, high-dose fish oil performed no better than placebo. Along these same lines, a 2022 systematic review and meta-analysis found the beneficial effects of these fats on epilepsy were most pronounced at doses of 1500 mg or less, and at durations of more than 16 weeks. This suggests that moderate omega-3 intake (realistically obtainable through diet) may be more therapeutic than high supplemental doses, at least where seizure conditions are concerned.
Additionally, a 2023 Mendelian randomization study, which helps discern cause and effect by combining genetic variation with epidemiology, revealed a causal relationship between blood levels of omega-3 fatty acids and the risk of epilepsy!
EPA and DHA and Osteoarthritis
Given their powerful anti-inflammatory effects, it might not be surprising that EPA and DHA can benefit osteoarthritis—a degenerative joint disease affecting cartilage and surrounding tissues. A 2023 meta-analysis of nine randomized controlled trials found that compared to placebo, supplementation with these fats could significantly improve arthritis pain and joint function. Several randomized controlled trials of EPA and DHA (in the form of fish oil) have shown that low doses are as effective, if not more effective, than higher doses in treating pain from osteoarthritis of the knee.
EPA and DHA and Sleep
EPA and DHA could even help improve sleep quality! A 2021 systematic review and meta-analysis, encompassing 20 randomized controlled trials and longitudinal studies, found that long-chain omega-3 fats can improve infants’ sleep organization and maturity—including reducing the wake-sleep transition, reducing the percentage of active sleep, and enhancing the percentage of wakefulness. Among children with clinical-level sleep problems, these fats can also reduce the total sleep disturbance score.
Although not all research has been consistent, some studies suggest adult sleep can benefit as well! A 2022 randomized controlled trial found that among healthy adults, 12 weeks of daily supplementation with EPA and DHA led to significant improvements in sleep quality, including more frequent dreaming and sleep efficiency. A 2022 analysis of National Health and Nutrition Examination Survey data likewise found that blood levels of long-chain omega-3 fats were associated with healthy sleep duration in adults.
EPA and DHA and Primary Sclerosing Cholangitis
Primary sclerosing cholangitis is a chronic liver disease that causes scarring and inflammation of the bile ducts, eventually resulting in them becoming narrow or blocked. And, long-chain omega-3 fats could be helpful for this condition!
In a 2013 pilot study of primary sclerosing cholangitis patients, 800 mg of DHA twice per day, for a period of 12 months, led to a significant decline in alkaline phosphatase levels (which become elevated from this condition). A 2021 study also found that the addition of EPA and DHA to ursodeoxycholic acid, the front-line treatment for certain liver disorders (including primary sclerosing cholangitis), strongly improved the therapeutic response compared to ursodeoxycholic acid alone. So, along with independently benefitting this condition, long-chain omega-3 fats could also make other treatments more effective!
The THREE Best Probiotics
Bacillus/Spore-based

Best for a general probiotic, if you were recently on antibiotics, or for digestion issues (especially abdominal pain, bloating, flatulence, diarrhea, and gas after meals).
Lactobacillus & Bifidobacterium

Best for if you don’t eat fermented foods, if you were recently on antibiotics, or if you have issues with constipation or gas.
Saccharomyces boulardii

Best for if you have Candida issues, were recently on antibiotics, or have diarrhea.
Health Effects of EPA and DHA Deficiency
A low intake of omega-3 fats in general, especially when omega-6 intake is simultaneously high, is associated with a greater risk of a number of health conditions developing over time (including cardiovascular disease, inflammatory skin conditions, and obesity). However, true omega-3 deficiency (and essential fatty acid deficiency in general) is very rare: even when intake or absorption is low—such as from being on a fat-restricted diet, or having a fat malabsorption disorder—the body is able to release essential fatty acids from fat tissue into circulation, preventing acute deficiency from occurring.
Documented cases of omega-3 deficiency are mostly limited to incidents from the 1970s and 1980s when people received parenteral nutrition (nutrients delivered intravenously) formulated without any polyunsaturated fatty acids, combined with glucose solutions that suppressed the release of essential fatty acids from fat tissue. In these cases, symptoms of classical essential fatty acid deficiency occurred in about 7 to 10 days, and included dry, scaly skin rashes and hair loss. Due to the role of omega-3s in maintaining proper nervous system functioning, chronic deficiency can also lead to numbness, leg pain, difficulty walking, poor growth in children, and blurred vision. But again, these effects are rare, and the biggest problem with omega-3 insufficiency is a higher long-term risk of chronic health issues, rather than any acute effects of deficiency.
Even when true deficiency doesn’t occur, though, insufficient EPA and DHA intake can have important effects on health. Skin irritation and dryness, mood disorders like depression, joint pain and stiffness, and dry eyes may be potential symptoms of inadequate intake—though the research here isn’t clear-cut, given the difficulty in defining cutoff levels for insufficiency. There’s also some evidence that inadequate omega-3 intake during pregnancy or in early life can increase the likelihood of learning disabilities, ADHD, and aggressive hostility.
Didn’t know EPA and DHA were this amazing? Maybe your friends will enjoy this too!
Problems From EPA and DHA Supplements
Importantly, along with these benefits, there are some potential problems associated with omega-3 supplements. In people with existing high cholesterol and triglycerides, omega-3 supplements—especially DHA—have sometimes been shown to increase LDL cholesterol by 5 to 10%. EPA has likewise been shown to increase bleeding time, and may interact with blood thinners in ways that enhance the activity of these drugs. Some studies have also found an increase in lipid peroxidation following fish oil supplementation, particularly when the doses are high and combined with activities that promote oxidative stress (such as endurance running). However, this may be due at least in part to the quality of the omega-3 supplements being used, and whether those supplements already contain oxidized lipids. In fact, in a variety of studies, between 11 and 80% of over-the-counter fish oil supplements have been shown to contain oxidized fats; in one study of American fish oil products, 27% had more than double the level of damage oxidized fats than the acceptable limit.
While this doesn’t mean that omega-3 supplements like fish oil are categorically dangerous, it does mean that sourcing high-quality products is important. Because the chemical structure of these fats are easily oxidized, they need to be extracted under ideal conditions, bottled and stored properly, and kept away from conditions that could drive oxidation (including higher temperatures, exposure to oxygen, exposure to light, exposure to water, and the presence of heavy metals). Some evidence also suggests that a higher vitamin E intake may be necessary to help offset the increased susceptibility to oxidative damage that comes with increased polyunsaturated fat intake (including omega-3 fats).
Everything You Need to Jump into Nutrivore TODAY!
Nutrivore Quickstart Guide
The Nutrivore Quickstart Guide e-book explains why and how to eat a Nutrivore diet, introduces the Nutrivore Score, gives a comprehensive tour of the full range of essential and important nutrients!
Plus, you’ll find the Top 100 Nutrivore Score Foods, analysis of food groups, practical tips to increase the nutrient density of your diet, and look-up tables for the Nutrivore Score of over 700 foods.
Buy now for instant digital access.
How Much EPA and DHA Do We Need?
The adequate intake level for omega-3 fats is 1.6 g daily for adult men and 1.1 g daily for adult women (1.4 g daily during pregnancy, and 1.3 g daily while breastfeeding), although there are currently no established dietary reference intakes specifically for EPA and DHA. The clinical benefits of omega-3 fats may require a higher intake than these guidelines.
Nutrient Daily Values
Nutrition requirements and recommended nutrient intake for infants, children, adolescents, adults, mature adults, and pregnant and lactating individuals.
Best Food Sources of EPA and DHA
The following foods have high concentrations of EPA and DHA, containing at least 125mg per serving, making them our best food sources of these crazy important omega-3 fats!
Want to know the top 500 most nutrient-dense foods?

Top 500 Nutrivore Foods
The Top 500 Nutrivore Foods e-book is an amazing reference deck of the top 500 most nutrient-dense foods according to their Nutrivore Score. Think of it as the go-to resource for a super-nerd, to learn more and better understand which foods stand out, and why!
If you are looking for a quick-reference guide to help enhance your diet with nutrients, and dive into the details of your favorite foods, this book is your one-stop-shop!
Buy now for instant digital access.
Good Food Sources of EPA and DHA
The following foods are also excellent or good sources of EPA and DHA, containing at least 25mg (and up to 125mg) per serving.
Citations
Expand to see all scientific references for this article.
Abdulrazaq M, Innes JK, Calder PC. Effect of ω-3 polyunsaturated fatty acids on arthritic pain: A systematic review. Nutrition. 2017 Jul-Aug;39-40:57-66. doi: 10.1016/j.nut.2016.12.003.
ADVANCE Collaborative Group, Patel A, MacMahon S, Chalmers J, Neal B, Billot L, Woodward M, Marre M, Cooper M, Glasziou P, Grobbee D, Hamet P, Harrap S, Heller S, Liu L, Mancia G, Mogensen CE, Pan C, Poulter N, Rodgers A, Williams B, Bompoint S, de Galan BE, Joshi R, Travert F. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008 Jun 12;358(24):2560-72. doi: 10.1056/NEJMoa0802987.
Aldhafiri FK. Investigating the Role of EPA and DHA on Cellular Oxidative Stress; Profiling Antidiabetic and Antihypertensive Potential. J Pharm Bioallied Sci. 2022 Oct-Dec;14(4):178-185. doi: 10.4103/jpbs.jpbs_383_22.
Aldoori J, Cockbain AJ, Toogood GJ, Hull MA. Omega-3 polyunsaturated fatty acids: moving towards precision use for prevention and treatment of colorectal cancer. Gut. 2022 Apr;71(4):822-837. doi: 10.1136/gutjnl-2021-326362.
Algarin YA, Pulumati A, Jaalouk D, Tan J, Nouri K. The role of vitamins and nutrients in rosacea. Arch Dermatol Res. 2024 May 2;316(5):142. doi: 10.1007/s00403-024-02895-4.
Alhassan A, Young J, Lean MEJ, Lara J. Consumption of fish and vascular risk factors: A systematic review and meta-analysis of intervention studies. Atherosclerosis. 2017 Nov;266:87-94. doi: 10.1016/j.atherosclerosis.2017.09.028.
Ameur A, Enroth S, Johansson A, Zaboli G, Igl W, Johansson AC, Rivas MA, Daly MJ, Schmitz G, Hicks AA, Meitinger T, Feuk L, van Duijn C, Oostra B, Pramstaller PP, Rudan I, Wright AF, Wilson JF, Campbell H, Gyllensten U. Genetic adaptation of fatty-acid metabolism: a human-specific haplotype increasing the biosynthesis of long-chain omega-3 and omega-6 fatty acids. Am J Hum Genet. 2012 May 4;90(5):809-20. doi: 10.1016/j.ajhg.2012.03.014.
Amminger GP, Schäfer MR, Papageorgiou K, Klier CM, Cotton SM, Harrigan SM, Mackinnon A, McGorry PD, Berger GE. Long-chain omega-3 fatty acids for indicated prevention of psychotic disorders: a randomized, placebo-controlled trial. Arch Gen Psychiatry. 2010 Feb;67(2):146-54. doi: 10.1001/archgenpsychiatry.2009.192.
Amminger GP, Schäfer MR, Schlögelhofer M, Klier CM, McGorry PD. Longer-term outcome in the prevention of psychotic disorders by the Vienna omega-3 study. Nat Commun. 2015 Aug 11;6:7934. doi: 10.1038/ncomms8934.
Ananthakrishnan AN, Khalili H, Konijeti GG, Higuchi LM, de Silva P, Fuchs CS, Willett WC, Richter JM, Chan AT. Long-term intake of dietary fat and risk of ulcerative colitis and Crohn’s disease. Gut. 2014 May;63(5):776-84. doi: 10.1136/gutjnl-2013-305304.
Arem H, Neuhouser ML, Irwin ML, Cartmel B, Lu L, Risch H, Mayne ST, Yu H. Omega-3 and omega-6 fatty acid intakes and endometrial cancer risk in a population-based case-control study. Eur J Nutr. 2013 Apr;52(3):1251-60. doi: 10.1007/s00394-012-0436-z.
ASCEND Study Collaborative Group, Bowman L, Mafham M, Wallendszus K, Stevens W, Buck G, Barton J, Murphy K, Aung T, Haynes R, Cox J, Murawska A, Young A, Lay M, Chen F, Sammons E, Waters E, Adler A, Bodansky J, Farmer A, McPherson R, Neil A, Simpson D, Peto R, Baigent C, Collins R, Parish S, Armitage J. Effects of n-3 Fatty Acid Supplements in Diabetes Mellitus. N Engl J Med. 2018 Oct 18;379(16):1540-1550. doi: 10.1056/NEJMoa1804989.
Attaman JA, Stanic AK, Kim M, Lynch MP, Rueda BR, Styer AK. The anti-inflammatory impact of omega-3 polyunsaturated Fatty acids during the establishment of endometriosis-like lesions. Am J Reprod Immunol. 2014 Oct;72(4):392-402. doi: 10.1111/aji.12276.
Aung T, Halsey J, Kromhout D, Gerstein HC, Marchioli R, Tavazzi L, Geleijnse JM, Rauch B, Ness A, Galan P, Chew EY, Bosch J, Collins R, Lewington S, Armitage J, Clarke R; Omega-3 Treatment Trialists’ Collaboration. Associations of Omega-3 Fatty Acid Supplement Use With Cardiovascular Disease Risks: Meta-analysis of 10 Trials Involving 77 917 Individuals. JAMA Cardiol. 2018 Mar 1;3(3):225-234. doi: 10.1001/jamacardio.2017.5205.
Bechthold A, Boeing H, Schwedhelm C, Hoffmann G, Knüppel S, Iqbal K, De Henauw S, Michels N, Devleesschauwer B, Schlesinger S, Schwingshackl L. Food groups and risk of coronary heart disease, stroke and heart failure: A systematic review and dose-response meta-analysis of prospective studies. Crit Rev Food Sci Nutr. 2019;59(7):1071-1090. doi: 10.1080/10408398.2017.1392288.
Beltz BS, Tlusty MF, Benton JL, Sandeman DC. Omega-3 fatty acids upregulate adult neurogenesis. Neurosci Lett. 2007 Mar 26;415(2):154-8. doi: 10.1016/j.neulet.2007.01.010.
Bhatt DL, Steg PG, Miller M, Brinton EA, Jacobson TA, Ketchum SB, Doyle RT Jr, Juliano RA, Jiao L, Granowitz C, Tardif JC, Ballantyne CM; REDUCE-IT Investigators. Cardiovascular Risk Reduction with Icosapent Ethyl for Hypertriglyceridemia. N Engl J Med. 2019 Jan 3;380(1):11-22. doi: 10.1056/NEJMoa1812792.
Brasky TM, Neuhouser ML, Cohn DE, White E. Associations of long-chain ω-3 fatty acids and fish intake with endometrial cancer risk in the VITamins And Lifestyle cohort. Am J Clin Nutr. 2014 Mar;99(3):599-608. doi: 10.3945/ajcn.113.070524.
Calder PC. n-3 fatty acids, inflammation and immunity: new mechanisms to explain old actions. Proc Nutr Soc. 2013 Aug;72(3):326-36. doi: 10.1017/S0029665113001031.
Calder PC. Polyunsaturated fatty acids and inflammatory processes: New twists in an old tale. Biochimie. 2009 Jun;91(6):791-5. doi: 10.1016/j.biochi.2009.01.008.
Caramia G. Gli acidi grassi essenziali omega-3 ed omega-6: dalla loro scoperta alle prospettive terapeutiche [The essential fatty acids omega-6 and omega-3: from their discovery to their use in therapy]. Minerva Pediatr. 2008 Apr;60(2):219-33.
Cardia L, Calapai F, Mondello C, Quattrone D, Elisa Sorbara E, Mannucci C, Calapai G, Mondello E. Clinical use of omega-3 fatty acids in migraine: A narrative review. Medicine (Baltimore). 2020 Oct 16;99(42):e22253. doi: 10.1097/MD.0000000000022253.
Carlson SE, Gajewski BJ, Alhayek S, Colombo J, Kerling EH, Gustafson KM. Dose-response relationship between docosahexaenoic acid (DHA) intake and lower rates of early preterm birth, low birth weight and very low birth weight. Prostaglandins Leukot Essent Fatty Acids. 2018 Nov;138:1-5. doi: 10.1016/j.plefa.2018.09.002.
Castro-Marrero J, Zaragozá MC, Domingo JC, Martinez-Martinez A, Alegre J, von Schacky C. Low omega-3 index and polyunsaturated fatty acid status in patients with chronic fatigue syndrome/myalgic encephalomyelitis. Prostaglandins Leukot Essent Fatty Acids. 2018 Dec;139:20-24. doi: 10.1016/j.plefa.2018.11.006.
Chan SS, Luben R, Olsen A, Tjonneland A, Kaaks R, Lindgren S, Grip O, Bergmann MM, Boeing H, Hallmans G, Karling P, Overvad K, Venø SK, van Schaik F, Bueno-de-Mesquita B, Oldenburg B, Khaw KT, Riboli E, Hart AR. Association between high dietary intake of the n-3 polyunsaturated fatty acid docosahexaenoic acid and reduced risk of Crohn’s disease. Aliment Pharmacol Ther. 2014 Apr;39(8):834-42. doi: 10.1111/apt.12670.
Chang JP, Su KP, Mondelli V, Satyanarayanan SK, Yang HT, Chiang YJ, Chen HT, Pariante CM. High-dose eicosapentaenoic acid (EPA) improves attention and vigilance in children and adolescents with attention deficit hyperactivity disorder (ADHD) and low endogenous EPA levels. Transl Psychiatry. 2019 Nov 20;9(1):303. doi: 10.1038/s41398-019-0633-0.
Chen C, Yu X, Shao S. Effects of Omega-3 Fatty Acid Supplementation on Glucose Control and Lipid Levels in Type 2 Diabetes: A Meta-Analysis. PLoS One. 2015 Oct 2;10(10):e0139565. doi: 10.1371/journal.pone.0139565.
Cockbain AJ, Toogood GJ, Hull MA. Omega-3 polyunsaturated fatty acids for the treatment and prevention of colorectal cancer. Gut. 2012 Jan;61(1):135-49. doi: 10.1136/gut.2010.233718.
Dai Y, Liu J. Omega-3 long-chain polyunsaturated fatty acid and sleep: a systematic review and meta-analysis of randomized controlled trials and longitudinal studies. Nutr Rev. 2021 Jul 7;79(8):847-868. doi: 10.1093/nutrit/nuaa103.
Das UN, Fams. Long-chain polyunsaturated fatty acids in the growth and development of the brain and memory. Nutrition. 2003 Jan;19(1):62-5. doi: 10.1016/s0899-9007(02)00852-3.
Das UN. Beneficial effect of eicosapentaenoic and docosahexaenoic acids in the management of systemic lupus erythematosus and its relationship to the cytokine network. Prostaglandins Leukot Essent Fatty Acids. 1994 Sep;51(3):207-13. doi: 10.1016/0952-3278(94)90136-8.
Davidson MH. Omega-3 fatty acids: new insights into the pharmacology and biology of docosahexaenoic acid, docosapentaenoic acid, and eicosapentaenoic acid. Curr Opin Lipidol. 2013 Dec;24(6):467-74. doi: 10.1097/MOL.0000000000000019.
DeGiorgio CM, Miller PR, Harper R, Gornbein J, Schrader L, Soss J, Meymandi S. Fish oil (n-3 fatty acids) in drug resistant epilepsy: a randomised placebo-controlled crossover study. J Neurol Neurosurg Psychiatry. 2015 Jan;86(1):65-70. doi: 10.1136/jnnp-2014-307749.
Del Gobbo LC, Imamura F, Aslibekyan S, Marklund M, Virtanen JK, Wennberg M, Yakoob MY, Chiuve SE, Dela Cruz L, Frazier-Wood AC, Fretts AM, Guallar E, Matsumoto C, Prem K, Tanaka T, Wu JH, Zhou X, Helmer C, Ingelsson E, Yuan JM, Barberger-Gateau P, Campos H, Chaves PH, Djoussé L, Giles GG, Gómez-Aracena J, Hodge AM, Hu FB, Jansson JH, Johansson I, Khaw KT, Koh WP, Lemaitre RN, Lind L, Luben RN, Rimm EB, Risérus U, Samieri C, Franks PW, Siscovick DS, Stampfer M, Steffen LM, Steffen BT, Tsai MY, van Dam RM, Voutilainen S, Willett WC, Woodward M, Mozaffarian D; Cohorts for Heart and Aging Research in Genomic Epidemiology (CHARGE) Fatty Acids and Outcomes Research Consortium (FORCe). ω-3 Polyunsaturated Fatty Acid Biomarkers and Coronary Heart Disease: Pooling Project of 19 Cohort Studies. JAMA Intern Med. 2016 Aug 1;176(8):1155-66. doi: 10.1001/jamainternmed.2016.2925.
Deng W, Yi Z, Yin E, Lu R, You H, Yuan X. Effect of omega-3 polyunsaturated fatty acids supplementation for patients with osteoarthritis: a meta-analysis. J Orthop Surg Res. 2023 May 24;18(1):381. doi: 10.1186/s13018-023-03855-w.
Djoussé L, Akinkuolie AO, Wu JH, Ding EL, Gaziano JM. Fish consumption, omega-3 fatty acids and risk of heart failure: a meta-analysis. Clin Nutr. 2012 Dec;31(6):846-53. doi: 10.1016/j.clnu.2012.05.010.
Donat-Vargas C, Berglund M, Glynn A, Wolk A, Åkesson A. Dietary polychlorinated biphenyls, long-chain n-3 polyunsaturated fatty acids and incidence of malignant melanoma. Eur J Cancer. 2017 Feb;72:137-143. doi: 10.1016/j.ejca.2016.11.016.
Duffy EM, Meenagh GK, McMillan SA, Strain JJ, Hannigan BM, Bell AL. The clinical effect of dietary supplementation with omega-3 fish oils and/or copper in systemic lupus erythematosus. J Rheumatol. 2004 Aug;31(8):1551-6.
Durán AM, Salto LM, Câmara J, Basu A, Paquien I, Beeson WL, Firek A, Cordero-MacIntyre Z, De León M. Effects of omega-3 polyunsaturated fatty-acid supplementation on neuropathic pain symptoms and sphingosine levels in Mexican-Americans with type 2 diabetes. Diabetes Metab Syndr Obes. 2019 Jan 8;12:109-120. doi: 10.2147/DMSO.S187268.
Egalini F, Guardamagna O, Gaggero G, Varaldo E, Giannone B, Beccuti G, Benso A, Broglio F. The Effects of Omega 3 and Omega 6 Fatty Acids on Glucose Metabolism: An Updated Review. Nutrients. 2023 Jun 8;15(12):2672. doi: 10.3390/nu15122672.
Fabian CJ, Kimler BF, Hursting SD. Omega-3 fatty acids for breast cancer prevention and survivorship. Breast Cancer Res. 2015 May 4;17(1):62. doi: 10.1186/s13058-015-0571-6.
Filaire E, Massart A, Portier H, Rouveix M, Rosado F, Bage AS, Gobert M, Durand D. Effect of 6 Weeks of n-3 fatty-acid supplementation on oxidative stress in Judo athletes. Int J Sport Nutr Exerc Metab. 2010 Dec;20(6):496-506. doi: 10.1123/ijsnem.20.6.496.
Fontani G, Corradeschi F, Felici A, Alfatti F, Migliorini S, Lodi L. Cognitive and physiological effects of Omega-3 polyunsaturated fatty acid supplementation in healthy subjects. Eur J Clin Invest. 2005 Nov;35(11):691-9. doi: 10.1111/j.1365-2362.2005.01570.x.
Fotuhi M, Mohassel P, Yaffe K. Fish consumption, long-chain omega-3 fatty acids and risk of cognitive decline or Alzheimer disease: a complex association. Nat Clin Pract Neurol. 2009 Mar;5(3):140-52. doi: 10.1038/ncpneuro1044.
Goh KK, Chen CY, Chen CH, Lu ML. Effects of omega-3 polyunsaturated fatty acids supplements on psychopathology and metabolic parameters in schizophrenia: A meta-analysis of randomized controlled trials. J Psychopharmacol. 2021 Mar;35(3):221-235. doi: 10.1177/0269881120981392.
Giosuè A, Calabrese I, Lupoli R, Riccardi G, Vaccaro O, Vitale M. Relations Between the Consumption of Fatty or Lean Fish and Risk of Cardiovascular Disease and All-cause Mortality: A Systematic Review and Meta-analysis. Adv Nutr. 2022 Feb 2:nmac006. doi: 10.1093/advances/nmac006.
Gioxari A, Kaliora AC, Marantidou F, Panagiotakos DP. Intake of ω-3 polyunsaturated fatty acids in patients with rheumatoid arthritis: A systematic review and meta-analysis. Nutrition. 2018 Jan;45:114-124.e4. doi: 10.1016/j.nut.2017.06.023.
Harel Z, Gascon G, Riggs S, Vaz R, Brown W, Exil G. Supplementation with omega-3 polyunsaturated fatty acids in the management of recurrent migraines in adolescents. J Adolesc Health. 2002 Aug;31(2):154-61. doi: 10.1016/s1054-139x(02)00349-x.
Harper CR, Edwards MJ, DeFilippis AP, Jacobson TA. Flaxseed oil increases the plasma concentrations of cardioprotective (n-3) fatty acids in humans. J Nutr. 2006 Jan;136(1):83-7. doi: 10.1093/jn/136.1.83.
Harris WS, Sands SA, Windsor SL, Ali HA, Stevens TL, Magalski A, Porter CB, Borkon AM. Omega-3 fatty acids in cardiac biopsies from heart transplantation patients: correlation with erythrocytes and response to supplementation. Circulation. 2004 Sep 21;110(12):1645-9. doi: 10.1161/01.CIR.0000142292.
He K, Song Y, Daviglus ML, Liu K, Van Horn L, Dyer AR, Greenland P. Accumulated evidence on fish consumption and coronary heart disease mortality: a meta-analysis of cohort studies. Circulation. 2004 Jun 8;109(22):2705-11. doi: 10.1161/01.CIR.0000132503.19410.6B.
Holman RT. The slow discovery of the importance of omega 3 essential fatty acids in human health. J Nutr. 1998 Feb;128(2 Suppl):427S-433S. doi: 10.1093/jn/128.2.427S.
Hopeman MM, Riley JK, Frolova AI, Jiang H, Jungheim ES. Serum Polyunsaturated Fatty Acids and Endometriosis. Reprod Sci. 2015 Sep;22(9):1083-7. doi: 10.1177/1933719114565030.
Ibrahim FAS, Ghebremeskel K, Abdel-Rahman ME, Ahmed AAM, Mohmed IM, Osman G, Elseed M, Hamed A, Rabinowicz AL, Salih MAM, Elbashir MI, Daak AA. The differential effects of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) on seizure frequency in patients with drug-resistant epilepsy – A randomized, double-blind, placebo-controlled trial. Epilepsy Behav. 2018 Oct;87:32-38. doi: 10.1016/j.yebeh.2018.08.016.
Jackson PA, Reay JL, Scholey AB, Kennedy DO. DHA-rich oil modulates the cerebral haemodynamic response to cognitive tasks in healthy young adults: a near IR spectroscopy pilot study. Br J Nutr. 2012 Apr;107(8):1093-8. doi: 10.1017/S0007114511004041.
Jayedi A, Zargar MS, Shab-Bidar S. Fish consumption and risk of myocardial infarction: a systematic review and dose-response meta-analysis suggests a regional difference. Nutr Res. 2019 Feb;62:1-12. doi: 10.1016/j.nutres.2018.10.009.
Jeffrey BG, Weisinger HS, Neuringer M, Mitchell DC. The role of docosahexaenoic acid in retinal function. Lipids. 2001 Sep;36(9):859-71. doi: 10.1007/s11745-001-0796-3.
Jump DB, Tripathy S, Depner CM. Fatty acid-regulated transcription factors in the liver. Annu Rev Nutr. 2013;33:249-69. doi: 10.1146/annurev-nutr-071812-161139.
Jump DB. The biochemistry of n-3 polyunsaturated fatty acids. J Biol Chem. 2002 Mar 15;277(11):8755-8. doi: 10.1074/jbc.R100062200.
Jung JY, Kwon HH, Hong JS, Yoon JY, Park MS, Jang MY, Suh DH. Effect of dietary supplementation with omega-3 fatty acid and gamma-linolenic acid on acne vulgaris: a randomised, double-blind, controlled trial. Acta Derm Venereol. 2014 Sep;94(5):521-5. doi: 10.2340/00015555-1802.
Jurkiewicz-Przondziono J, Lemm M, Kwiatkowska-Pamuła A, Ziółko E, Wójtowicz MK. Influence of diet on the risk of developing endometriosis. Ginekol Pol. 2017;88(2):96-102. doi: 10.5603/GP.a2017.0017.
Kang JI, Yoon HS, Kim SM, Park JE, Hyun YJ, Ko A, Ahn YS, Koh YS, Hyun JW, Yoo ES, Kang HK. Mackerel-Derived Fermented Fish Oil Promotes Hair Growth by Anagen-Stimulating Pathways. Int J Mol Sci. 2018 Sep 14;19(9):2770. doi: 10.3390/ijms19092770.
Kar S, Wong M, Rogozinska E, Thangaratinam S. Effects of omega-3 fatty acids in prevention of early preterm delivery: a systematic review and meta-analysis of randomized studies. Eur J Obstet Gynecol Reprod Biol. 2016 Mar;198:40-46. doi: 10.1016/j.ejogrb.2015.11.033.
Khanaki K, Nouri M, Ardekani AM, Ghassemzadeh A, Shahnazi V, Sadeghi MR, Darabi M, Mehdizadeh A, Dolatkhah H, Saremi A, Imani AR, Rahimipour A. Evaluation of the relationship between endometriosis and omega-3 and omega-6 polyunsaturated fatty acids. Iran Biomed J. 2012;16(1):38-43. doi: 10.6091/ibj.1025.2012.
Kiecolt-Glaser JK, Belury MA, Andridge R, Malarkey WB, Glaser R. Omega-3 supplementation lowers inflammation and anxiety in medical students: a randomized controlled trial. Brain Behav Immun. 2011 Nov;25(8):1725-34. doi: 10.1016/j.bbi.2011.07.229.
Kim EJ, Kim MK, Jin XJ, Oh JH, Kim JE, Chung JH. Skin aging and photoaging alter fatty acids composition, including 11,14,17-eicosatrienoic acid, in the epidermis of human skin. J Korean Med Sci. 2010 Jun;25(6):980-3. doi: 10.3346/jkms.2010.25.6.980.
Kitson AP, Stroud CK, Stark KD. Elevated production of docosahexaenoic acid in females: potential molecular mechanisms. Lipids. 2010 Mar;45(3):209-24. doi: 10.1007/s11745-010-3391-6.
Krittanawong C, Isath A, Hahn J, Wang Z, Narasimhan B, Kaplin SL, Jneid H, Virani SS, Tang WHW. Fish Consumption and Cardiovascular Health: A Systematic Review. Am J Med. 2021 Jun;134(6):713-720. doi: 10.1016/j.amjmed.2020.12.017.
Le Floc’h C, Cheniti A, Connétable S, Piccardi N, Vincenzi C, Tosti A. Effect of a nutritional supplement on hair loss in women. J Cosmet Dermatol. 2015 Mar;14(1):76-82. doi: 10.1111/jocd.12127.
Lembke P, Capodice J, Hebert K, Swenson T. Influence of omega-3 (n3) index on performance and wellbeing in young adults after heavy eccentric exercise. J Sports Sci Med. 2014 Jan 20;13(1):151-6.
Lewis EJH, Lovblom LE, Cisbani G, Chen DK, Bazinet RP, Wolever TMS, Perkins BA, Bril V. Baseline omega-3 level is associated with nerve regeneration following 12-months of omega-3 nutrition therapy in patients with type 1 diabetes. J Diabetes Complications. 2021 Mar;35(3):107798. doi: 10.1016/j.jdiacomp.2020.107798.
Liang Z, Lou Y, Li Z, Liu S. Causal relationship between human blood omega-3 fatty acids and the risk of epilepsy: A two-sample Mendelian randomization study. Front Neurol. 2023 Mar 9;14:1130439. doi: 10.3389/fneur.2023.1130439.
Liao Y, Xie B, Zhang H, He Q, Guo L, Subramanieapillai M, Fan B, Lu C, McIntyre RS. Efficacy of omega-3 PUFAs in depression: A meta-analysis. Transl Psychiatry. 2019 Aug 5;9(1):190. doi: 10.1038/s41398-019-0515-5.
Linseisen J, Grundmann N, Zoller D, Kühn T, Jansen EHJM, Chajès V, Fedirko V, Weiderpass E, Dahm CC, Overvad K, Tjønneland A, Boutron-Ruault MC, Rothwell JA, Severi G, Kaaks R, Schulze MB, Aleksandrova K, Sieri S, Panico S, Tumino R, Masala G, De Marco L, Bueno-de-Mesquita B, Vermeulen R, Gram IT, Skeie G, Chirlaque MD, Ardanaz E, Agudo A, Sánchez MJ, Amiano P, Wennberg M, Bodén S, Perez-Cornago A, Aglago EK, Gunter MJ, Jenab M, Heath AK, Nieters A. Red Blood Cell Fatty Acids and Risk of Colorectal Cancer in The European Prospective Investigation into Cancer and Nutrition (EPIC). Cancer Epidemiol Biomarkers Prev. 2021 May;30(5):874-885. doi: 10.1158/1055-9965.EPI-20-1426.
Logan SL, Spriet LL. Omega-3 Fatty Acid Supplementation for 12 Weeks Increases Resting and Exercise Metabolic Rate in Healthy Community-Dwelling Older Females. PLoS One. 2015 Dec 17;10(12):e0144828. doi: 10.1371/journal.pone.0144828.
Lu Y, Li D, Wang L, Zhang H, Jiang F, Zhang R, Xu L, Yang N, Dai S, Xu X, Theodoratou E, Li X. Comprehensive Investigation on Associations between Dietary Intake and Blood Levels of Fatty Acids and Colorectal Cancer Risk. Nutrients. 2023 Feb 1;15(3):730. doi: 10.3390/nu15030730.
Ma Y, Wang J, Li Q, Cao B. The Effect of Omega-3 Polyunsaturated Fatty Acid Supplementations on anti-Tumor Drugs in Triple Negative Breast Cancer. Nutr Cancer. 2021;73(2):196-205. doi: 10.1080/01635581.2020.1743873.
Maghsoumi-Norouzabad L, Mansoori A, Abed R, Shishehbor F. Effects of omega-3 fatty acids on the frequency, severity, and duration of migraine attacks: A systematic review and meta-analysis of randomized controlled trials. Nutr Neurosci. 2018 Nov;21(9):614-623. doi: 10.1080/1028415X.2017.1344371.
Maes M, Mihaylova I, Leunis JC. In chronic fatigue syndrome, the decreased levels of omega-3 poly-unsaturated fatty acids are related to lowered serum zinc and defects in T cell activation. Neuro Endocrinol Lett. 2005 Dec;26(6):745-51.
Manson JE, Cook NR, Lee IM, Christen W, Bassuk SS, Mora S, Gibson H, Albert CM, Gordon D, Copeland T, D’Agostino D, Friedenberg G, Ridge C, Bubes V, Giovannucci EL, Willett WC, Buring JE; VITAL Research Group. Marine n-3 Fatty Acids and Prevention of Cardiovascular Disease and Cancer. N Engl J Med. 2019 Jan 3;380(1):23-32. doi: 10.1056/NEJMoa1811403.
Marcinkowska A, Górnicka M. The Role of Dietary Fats in the Development and Treatment of Endometriosis. Life (Basel). 2023 Feb 27;13(3):654. doi: 10.3390/life13030654.
Martin CR, Blanco PG, Keach JC, Petz JL, Zaman MM, Bhaskar KR, Cluette-Brown JE, Gautam S, Sheth S, Afdhal NH, Lindor KD, Freedman SD. The safety and efficacy of oral docosahexaenoic acid supplementation for the treatment of primary sclerosing cholangitis – a pilot study. Aliment Pharmacol Ther. 2012 Jan;35(2):255-65. doi: 10.1111/j.1365-2036.2011.04926.x.
Marton LT, Goulart RA, Carvalho ACA, Barbalho SM. Omega Fatty Acids and Inflammatory Bowel Diseases: An Overview. Int J Mol Sci. 2019 Sep 30;20(19):4851. doi: 10.3390/ijms20194851.
McLennan PL. Cardiac physiology and clinical efficacy of dietary fish oil clarified through cellular mechanisms of omega-3 polyunsaturated fatty acids. Eur J Appl Physiol. 2014;114(7):1333-56. doi: 10.1007/s00421-014-2876-z.
Metherel AH, Irfan M, Klingel SL, Mutch DM, Bazinet RP. Compound-specific isotope analysis reveals no retroconversion of DHA to EPA but substantial conversion of EPA to DHA following supplementation: a randomized control trial. Am J Clin Nutr. 2019 Oct 1;110(4):823-831. doi: 10.1093/ajcn/nqz097.
Missmer SA, Chavarro JE, Malspeis S, Bertone-Johnson ER, Hornstein MD, Spiegelman D, Barbieri RL, Willett WC, Hankinson SE. A prospective study of dietary fat consumption and endometriosis risk. Hum Reprod. 2010 Jun;25(6):1528-35. doi: 10.1093/humrep/deq044.
Miura K, Way M, Jiyad Z, Marquart L, Plasmeijer EI, Campbell S, Isbel N, Fawcett J, Ferguson LE, Davis M, Whiteman DC, Soyer HP, O’Rourke P, Green AC. Omega-3 fatty acid intake and decreased risk of skin cancer in organ transplant recipients. Eur J Nutr. 2021 Jun;60(4):1897-1905. doi: 10.1007/s00394-020-02378-y.
Mozaffarian D, Wu JH. Omega-3 fatty acids and cardiovascular disease: effects on risk factors, molecular pathways, and clinical events. J Am Coll Cardiol. 2011 Nov 8;58(20):2047-67. doi: 10.1016/j.jacc.2011.06.063.
Murphy RA, Devarshi PP, Mun JG, Marshall K, Mitmesser SH. Association of omega-3 levels and sleep in US adults, National Health and Nutrition Examination Survey, 2011-2012. Sleep Health. 2022 Jun;8(3):294-297. doi: 10.1016/j.sleh.2021.12.003.
Nahab F, Pearson K, Frankel MR, Ard J, Safford MM, Kleindorfer D, Howard VJ, Judd S. Dietary fried fish intake increases risk of CVD: the REasons for Geographic And Racial Differences in Stroke (REGARDS) study. Public Health Nutr. 2016 Dec;19(18):3327-3336. doi: 10.1017/S136898001600152X.
Narendran R, Frankle WG, Mason NS, Muldoon MF, Moghaddam B. Improved working memory but no effect on striatal vesicular monoamine transporter type 2 after omega-3 polyunsaturated fatty acid supplementation. PLoS One. 2012;7(10):e46832. doi: 10.1371/journal.pone.0046832.
Ogawa S, Abe T, Nako K, Okamura M, Senda M, Sakamoto T, Ito S; DIMS Study Group. Eicosapentaenoic acid improves glycemic control in elderly bedridden patients with type 2 diabetes. Tohoku J Exp Med. 2013;231(1):63-74. doi: 10.1620/tjem.231.63.
Okuda Y, Mizutani M, Ogawa M, Sone H, Asano M, Asakura Y, Isaka M, Suzuki S, Kawakami Y, Field JB, Yamashita K. Long-term effects of eicosapentaenoic acid on diabetic peripheral neuropathy and serum lipids in patients with type II diabetes mellitus. J Diabetes Complications. 1996 Sep-Oct;10(5):280-7. doi: 10.1016/1056-8727(95)00081-x.
Osouli-Tabrizi S, Mehdizadeh A, Naghdi M, Sanaat Z, Vahed N, Farshbaf-Khalili A. The effectiveness of omega-3 fatty acids on health outcomes in women with breast cancer: A systematic review. Food Sci Nutr. 2023 May 22;11(8):4355-4371. doi: 10.1002/fsn3.3409.
Paixão EMDS, Oliveira ACM, Pizato N, Muniz-Junqueira MI, Magalhães KG, Nakano EY, Ito MK. The effects of EPA and DHA enriched fish oil on nutritional and immunological markers of treatment naïve breast cancer patients: a randomized double-blind controlled trial. Nutr J. 2017 Oct 23;16(1):71. doi: 10.1186/s12937-017-0295-9.
Patterson E, Wall R, Fitzgerald GF, Ross RP, Stanton C. Health implications of high dietary omega-6 polyunsaturated Fatty acids. J Nutr Metab. 2012;2012:539426. doi: 10.1155/2012/539426.
Puri BK. The use of eicosapentaenoic acid in the treatment of chronic fatigue syndrome. Prostaglandins Leukot Essent Fatty Acids. 2004 Apr;70(4):399-401. doi: 10.1016/j.plefa.2003.12.015.
Rimm EB, Appel LJ, Chiuve SE, Djoussé L, Engler MB, Kris-Etherton PM, Mozaffarian D, Siscovick DS, Lichtenstein AH; American Heart Association Nutrition Committee of the Council on Lifestyle and Cardiometabolic Health; Council on Epidemiology and Prevention; Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; and Council on Clinical Cardiology. Seafood Long-Chain n-3 Polyunsaturated Fatty Acids and Cardiovascular Disease: A Science Advisory From the American Heart Association. Circulation. 2018 Jul 3;138(1):e35-e47. doi: 10.1161/CIR.0000000000000574.
Rizos EC, Markozannes G, Tsapas A, Mantzoros CS, Ntzani EE. Omega-3 supplementation and cardiovascular disease: formulation-based systematic review and meta-analysis with trial sequential analysis. Heart. 2021 Jan;107(2):150-158. doi: 10.1136/heartjnl-2020-316780.
Romano C, Cucchiara S, Barabino A, Annese V, Sferlazzas C. Usefulness of omega-3 fatty acid supplementation in addition to mesalazine in maintaining remission in pediatric Crohn’s disease: a double-blind, randomized, placebo-controlled study. World J Gastroenterol. 2005 Dec 7;11(45):7118-21. doi: 10.3748/wjg.v11.i45.7118.
Sanders AE, Shaikh SR, Slade GD. Long-chain omega-3 fatty acids and headache in the U.S. population. Prostaglandins Leukot Essent Fatty Acids. 2018 Aug;135:47-53. doi: 10.1016/j.plefa.2018.06.008.
Samieri C, Morris MC, Bennett DA, Berr C, Amouyel P, Dartigues JF, Tzourio C, Chasman DI, Grodstein F. Fish Intake, Genetic Predisposition to Alzheimer Disease, and Decline in Global Cognition and Memory in 5 Cohorts of Older Persons. Am J Epidemiol. 2018 May 1;187(5):933-940. doi: 10.1093/aje/kwx330.
Samimi M, Jamilian M, Asemi Z, Esmaillzadeh A. Effects of omega-3 fatty acid supplementation on insulin metabolism and lipid profiles in gestational diabetes: Randomized, double-blind, placebo-controlled trial. Clin Nutr. 2015 Jun;34(3):388-93. doi: 10.1016/j.clnu.2014.06.005.
SanGiovanni JP, Chew EY. The role of omega-3 long-chain polyunsaturated fatty acids in health and disease of the retina. Prog Retin Eye Res. 2005 Jan;24(1):87-138. doi: 10.1016/j.preteyeres.2004.06.002.
Sarbolouki S, Javanbakht MH, Derakhshanian H, Hosseinzadeh P, Zareei M, Hashemi SB, Dorosty AR, Eshraghian MR, Djalali M. Eicosapentaenoic acid improves insulin sensitivity and blood sugar in overweight type 2 diabetes mellitus patients: a double-blind randomised clinical trial. Singapore Med J. 2013 Jul;54(7):387-90. doi: 10.11622/smedj.2013139.
Senapati S, Gragg M, Samuels IS, Parmar VM, Maeda A, Park PS. Effect of dietary docosahexaenoic acid on rhodopsin content and packing in photoreceptor cell membranes. Biochim Biophys Acta Biomembr. 2018 Jun;1860(6):1403-1413. doi: 10.1016/j.bbamem.2018.03.030.
Shimura T, Miura T, Usami M, Ishihara E, Tanigawa K, Ishida H, Seino Y. Docosahexanoic acid (DHA) improved glucose and lipid metabolism in KK-Ay mice with genetic non-insulin-dependent diabetes mellitus (NIDDM). Biol Pharm Bull. 1997 May;20(5):507-10. doi: 10.1248/bpb.20.507.
Simopoulos AP. An Increase in the Omega-6/Omega-3 Fatty Acid Ratio Increases the Risk for Obesity. Nutrients. 2016 Mar 2;8(3):128. doi: 10.3390/nu8030128.
So J, Wu D, Lichtenstein AH, Tai AK, Matthan NR, Maddipati KR, Lamon-Fava S. EPA and DHA differentially modulate monocyte inflammatory response in subjects with chronic inflammation in part via plasma specialized pro-resolving lipid mediators: A randomized, double-blind, crossover study. Atherosclerosis. 2021 Jan;316:90-98. doi: 10.1016/j.atherosclerosis.2020.11.018.
Song M, Lee IM, Manson JE, Buring JE, Dushkes R, Gordon D, Walter J, Wu K, Chan AT, Ogino S, Fuchs CS, Meyerhardt JA, Giovannucci EL; VITAL Research Group. Effect of Supplementation With Marine ω-3 Fatty Acid on Risk of Colorectal Adenomas and Serrated Polyps in the US General Population: A Prespecified Ancillary Study of a Randomized Clinical Trial. JAMA Oncol. 2020 Jan 1;6(1):108-115. doi: 10.1001/jamaoncol.2019.4587.
Sperling LS, Nelson JR. History and future of omega-3 fatty acids in cardiovascular disease. Curr Med Res Opin. 2016;32(2):301-11. doi: 10.1185/03007995.2015.1120190.
Stillwell W, Wassall SR. Docosahexaenoic acid: membrane properties of a unique fatty acid. Chem Phys Lipids. 2003 Nov;126(1):1-27. doi: 10.1016/s0009-3084(03)00101-4.
Su KP, Tseng PT, Lin PY, Okubo R, Chen TY, Chen YW, Matsuoka YJ. Association of Use of Omega-3 Polyunsaturated Fatty Acids With Changes in Severity of Anxiety Symptoms: A Systematic Review and Meta-analysis. JAMA Netw Open. 2018 Sep 7;1(5):e182327. doi: 10.1001/jamanetworkopen.2018.2327.
Swanson D, Block R, Mousa SA. Omega-3 fatty acids EPA and DHA: health benefits throughout life. Adv Nutr. 2012 Jan;3(1):1-7. doi: 10.3945/an.111.000893.
Tanaka K, Ishikawa Y, Yokoyama M, Origasa H, Matsuzaki M, Saito Y, Matsuzawa Y, Sasaki J, Oikawa S, Hishida H, Itakura H, Kita T, Kitabatake A, Nakaya N, Sakata T, Shimada K, Shirato K; JELIS Investigators, Japan. Reduction in the recurrence of stroke by eicosapentaenoic acid for hypercholesterolemic patients: subanalysis of the JELIS trial. Stroke. 2008 Jul;39(7):2052-8. doi: 10.1161/STROKEAHA.107.509455.
Teisen MN, Vuholm S, Niclasen J, Aristizabal-Henao JJ, Stark KD, Geertsen SS, Damsgaard CT, Lauritzen L. Effects of oily fish intake on cognitive and socioemotional function in healthy 8-9-year-old children: the FiSK Junior randomized trial. Am J Clin Nutr. 2020 Jul 1;112(1):74-83. doi: 10.1093/ajcn/nqaa050.
Therdyothin A, Phiphopthatsanee N, Isanejad M. The Effect of Omega-3 Fatty Acids on Sarcopenia: Mechanism of Action and Potential Efficacy. Mar Drugs. 2023 Jul 13;21(7):399. doi: 10.3390/md21070399.
Thérien A, Cieślak A, Verreault M, Perreault M, Trottier J, Gobeil S, Vohl MC, Barbier O. Omega-3 Polyunsaturated Fatty Acid: A Pharmaco-Nutraceutical Approach to Improve the Responsiveness to Ursodeoxycholic Acid. Nutrients. 2021 Jul 29;13(8):2617. doi: 10.3390/nu13082617.
Thomsen BJ, Chow EY, Sapijaszko MJ. The Potential Uses of Omega-3 Fatty Acids in Dermatology: A Review. J Cutan Med Surg. 2020 Sep/Oct;24(5):481-494. doi: 10.1177/1203475420929925.
Tomaszewski N, He X, Solomon V, Lee M, Mack WJ, Quinn JF, Braskie MN, Yassine HN. Effect of APOE Genotype on Plasma Docosahexaenoic Acid (DHA), Eicosapentaenoic Acid, Arachidonic Acid, and Hippocampal Volume in the Alzheimer’s Disease Cooperative Study-Sponsored DHA Clinical Trial. J Alzheimers Dis. 2020;74(3):975-990. doi: 10.3233/JAD-191017.
Wang C, Harris WS, Chung M, Lichtenstein AH, Balk EM, Kupelnick B, Jordan HS, Lau J. n-3 Fatty acids from fish or fish-oil supplements, but not alpha-linolenic acid, benefit cardiovascular disease outcomes in primary- and secondary-prevention studies: a systematic review. Am J Clin Nutr. 2006 Jul;84(1):5-17. doi: 10.1093/ajcn/84.1.5.
Wang J, Zhang Y, Zhao L. Omega-3 PUFA intake and the risk of digestive system cancers: A meta-analysis of observational studies. Medicine (Baltimore). 2020 May;99(19):e20119. doi: 10.1097/MD.0000000000020119.
Wani AL, Bhat SA, Ara A. Omega-3 fatty acids and the treatment of depression: a review of scientific evidence. Integr Med Res. 2015 Sep;4(3):132-141. doi: 10.1016/j.imr.2015.07.003.
Westberg G, Tarkowski A. Effect of MaxEPA in patients with SLE. A double-blind, crossover study. Scand J Rheumatol. 1990;19(2):137-43. doi: 10.3109/03009749009102117.
Wolters M, von der Haar A, Baalmann AK, Wellbrock M, Heise TL, Rach S. Effects of n-3 Polyunsaturated Fatty Acid Supplementation in the Prevention and Treatment of Depressive Disorders-A Systematic Review and Meta-Analysis. Nutrients. 2021 Mar 25;13(4):1070. doi: 10.3390/nu13041070.
Wright SA, O’Prey FM, McHenry MT, Leahey WJ, Devine AB, Duffy EM, Johnston DG, Finch MB, Bell AL, McVeigh GE. A randomised interventional trial of omega-3-polyunsaturated fatty acids on endothelial function and disease activity in systemic lupus erythematosus. Ann Rheum Dis. 2008 Jun;67(6):841-8. doi: 10.1136/ard.2007.077156.
Xu D, Lu Y, Yang X, Pan D, Wang Y, Yin S, Wang S, Sun G. Effects of fish oil-derived n-3 polyunsaturated fatty acid on body composition, muscle strength and physical performance in older people: a secondary analysis of a randomised, double-blind, placebo-controlled trial. Age Ageing. 2022 Dec 5;51(12):afac274. doi: 10.1093/ageing/afac274.
Yokoyama M, Origasa H, Matsuzaki M, Matsuzawa Y, Saito Y, Ishikawa Y, Oikawa S, Sasaki J, Hishida H, Itakura H, Kita T, Kitabatake A, Nakaya N, Sakata T, Shimada K, Shirato K; Japan EPA lipid intervention study (JELIS) Investigators. Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (JELIS): a randomised open-label, blinded endpoint analysis. Lancet. 2007 Mar 31;369(9567):1090-8. doi: 10.1016/S0140-6736(07)60527-3.
Yurko-Mauro K, McCarthy D, Rom D, Nelson EB, Ryan AS, Blackwell A, Salem N Jr, Stedman M; MIDAS Investigators. Beneficial effects of docosahexaenoic acid on cognition in age-related cognitive decline. Alzheimers Dement. 2010 Nov;6(6):456-64. doi: 10.1016/j.jalz.2010.01.013.
Zhang Y, Chen J, Qiu J, Li Y, Wang J, Jiao J. Intakes of fish and polyunsaturated fatty acids and mild-to-severe cognitive impairment risks: a dose-response meta-analysis of 21 cohort studies. Am J Clin Nutr. 2016 Feb;103(2):330-40. doi: 10.3945/ajcn.115.124081.
Zhao LG, Sun JW, Yang Y, Ma X, Wang YY, Xiang YB. Fish consumption and all-cause mortality: a meta-analysis of cohort studies. Eur J Clin Nutr. 2016 Feb;70(2):155-61. doi: 10.1038/ejcn.2015.72.
Zheng T, Zhao J, Wang Y, Liu W, Wang Z, Shang Y, Zhang W, Zhang Y, Zhong M. The limited effect of omega-3 polyunsaturated fatty acids on cardiovascular risk in patients with impaired glucose metabolism: a meta-analysis. Clin Biochem. 2014 Apr;47(6):369-77. doi: 10.1016/j.clinbiochem.2013.11.025. Epub 2013 Dec 14.
Ready to Make Healthy Eating Feel Effortless?
Join the FREE 90-day Nutrivore90 Challenge and build lasting habits with no food rules, no guilt—just real progress.
- Weekly downloads, journal prompts, and reflection tools—all completely free.
- Focus on nutrient density, not restriction
- Starts September 1st!