Headaches and migraines are neurological conditions that significantly impact the lives of many individuals in the United States. A headache is characterized by pain in any region of the head, varying in intensity, duration, and cause. Migraines, however, are a specific type of headache disorder marked by recurrent episodes of severe, throbbing pain in which episodes often accompany nausea, vomiting, and heightened sensitivity to light and sound. Some individuals may experience an “aura” before the onset of a migraine, involving visual disturbances or tingling sensations.
Migraines and severe headaches are common in the U.S., affecting a substantial portion of the population. According to the Centers for Disease Control and Prevention (CDC), in 2018, 20.0% of women and 9.7% of men reported experiencing a severe headache or migraine in the past three months. The prevalence was highest among individuals aged 18–44 years and tended to decrease with age.
What Are Causes and Risk Factors of Headaches & Migraines?
The exact mechanisms behind headaches and migraine headaches are complex and not entirely understood. Migraines are believed to involve genetic and environmental factors leading to abnormal brain activity and affecting nerve signaling, neurotransmitters, and blood vessels in the brain. Common migraine triggers include hormonal fluctuations, certain foods and beverages, stress, sensory stimuli, changes in sleep patterns, physical exertion, and environmental changes.
Several factors may increase the likelihood of developing migraines:
- Genetics: A family history of migraines increases the risk, suggesting a hereditary component.
- Age: Migraines often begin during adolescence and are most prevalent in individuals between 18 and 44 years old.
- Sex: Women are more likely than men to experience migraines, partly due to hormonal influences.
- Hormonal Changes: Fluctuations in estrogen levels, such as those occurring during menstruation, pregnancy, or menopause, can trigger migraines in some women.
How Do You Reduce Risk of Headaches & Migraines?

To minimize the frequency and severity of headaches and migraines, the following considerations can be taken into account:
- Maintain a Regular Sleep Schedule: Aim for consistent sleep patterns, as both insufficient and excessive sleep can provoke migraines.
- Identify and Avoid Triggers: Maintain a headache diary to recognize patterns and specific triggers, such as certain foods, stressors, or environmental factors.
- Manage Stress: Engage in relaxation techniques like meditation, yoga, or deep-breathing exercises to reduce stress levels.
- Exercise Regularly: Incorporate moderate physical activity into your routine, as regular exercise can help decrease migraine frequency.
- Monitor Diet: Be mindful of dietary choices, avoiding known food triggers such as aged cheeses, processed meats, and alcohol.
- Stay Hydrated: Ensure adequate hydration, as dehydration can lead to headaches.
- Limit Caffeine Intake: Moderate caffeine consumption, as both excessive intake and withdrawal can trigger headaches.
- Consult a Healthcare Provider: If migraines are frequent or severe, seek medical advice. Preventive medications or therapies may be appropriate.
Nutrients for Headaches & Migraines
Learn more about all of the nutrients linked to risk of headaches and migraines, the other ways these nutrients improve our health, and the best food sources of each of them!
How Do Nutrients Improve Headaches & Migraines?
A Nutrivore approach emphasizes nutrients that help the body function at its best—including the systems involved in neurological signaling, inflammation, and pain regulation. Current research highlights the following nutrients for supporting headaches and migraines, along with food sources to help you incorporate these nutrients through your diet.
| Nutrient | How it Supports Headaches & Migraines | Top Food Sources |
|---|---|---|
| Vitamin B2 (Riboflavin) | Riboflavin may reduce migraine frequency and severity by supporting mitochondrial energy production; impaired mitochondrial oxygen metabolism is believed to play a role in migraine development. It is also sometimes used for pediatric migraines, though with mixed results. | Top food sources include organ meat, mushrooms, leafy green vegetables, eggs, milk and other dairy products, almonds, yeast, legumes, and squash. |
| CoQ10 | CoQ10 supplementation has been shown to reduce the number of monthly migraine days, shorten migraine duration, and lessen migraine severity in both adults and children, likely through improved mitochondrial function and reduced oxidative stress. | Top food sources include fatty fish (salmon, mackerel, yellowtail, trout, sardines), organ meats (heart, liver, kidney), beef, chicken, pork, Brassica vegetables, legumes, peanuts, nuts, and seeds. |
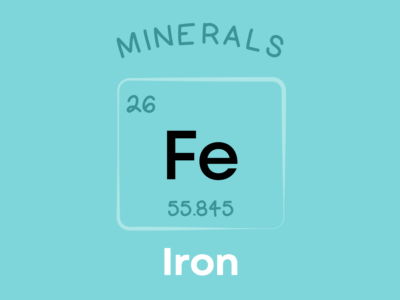
| Iron | Iron deficiency is associated with higher migraine risk in women, particularly menstrual and menstrually related migraines; low hemoglobin and ferritin levels may worsen susceptibility. Dietary iron intake is inversely linked with severe headaches in premenopausal women. | Top food sources include liver, red meat, oysters, mussels, clams, dark leafy greens, legumes such as lentils and kidney beans, peas, white beans, chickpeas, and blackstrap molasses. |
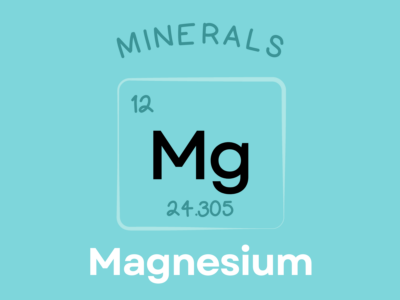
| Magnesium | Magnesium may prevent migraine attacks by reducing cortical spreading depression—a wave of altered brain activity that often precedes migraines—and supplementation of 400–500 mg/day has shown benefit in clinical studies. | Top food sources include leafy greens, nuts and seeds (especially pumpkin seeds, almonds, and cashews), fish, legumes, whole grains, cocoa, avocados, spices, and low-fat dairy products like milk and yogurt. |
| Zinc | Higher zinc intake is associated with significantly reduced migraine risk, and supplementation has been shown to reduce migraine frequency and severity, potentially through anti-inflammatory and antioxidant effects. | Top food sources include red meat, organ meats (liver, heart), seafood (especially oysters), eggs, legumes, nuts, and whole grains. |
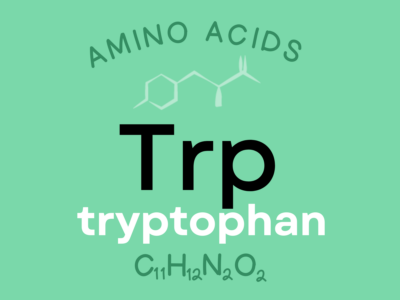
| Tryptophan | Higher tryptophan intake is associated with markedly lower migraine risk, though research is still limited. Effects may occur via serotonin pathways, given tryptophan’s role as its precursor. | Top food sources include poultry, egg whites, dairy, seeds such as sunflower, pumpkin, and sesame, soybeans, peanuts, oats, bananas, and fish. |
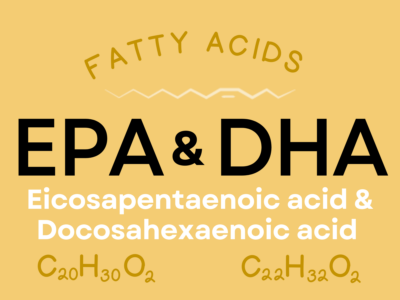
| EPA & DHA | Higher intake of omega-3 fatty acids like EPA and DHA is associated with lower headache prevalence, and supplementation can significantly reduce migraine duration—likely due to anti-inflammatory and neuroprotective effects on pain pathways. | Top food sources include fatty cold-water fish like salmon, herring, mackerel, sardines, and menhaden, as well as some algae, cod liver oil, and shellfish including mussels, crab, oysters, and squid. |

Nutrients for Headaches & Migraines
Nutrients for Headaches & Migraines explains the nutrients that matter most for headache frequency, migraine risk, and brain health! This e-book is exclusively available in Patreon!
Plus every month, you’ll gain exclusive and early access to a variety of resources, including a weekly video podcast, a new e-book in a series, nutrient fun factsheet, and more! Sign up now and also get 5 free Nutrivore guides as a welcome gift! Win-win-win!
Benefits of a Food-Based Approach

A nutrient-focused, whole-food approach can play a supportive role in managing many health conditions, especially when paired with healthy lifestyle habits like physical activity and good-quality sleep. A food-based approach to nutrition offers health benefits that go far beyond what supplements can provide. Whole foods deliver a natural balance of nutrients that work synergistically, meaning vitamins, minerals, phytonutrients, healthy fats, carbohydrates and fiber can support each other for better overall health outcomes. Nutrient-dense foods like leafy greens, fruits, legumes, nuts, seeds, and fish are efficient, cost-effective, and widely accessible options that fit easily into a healthy diet and good eating patterns. By choosing whole foods first, you not only support a more balanced diet but also avoid the added costs and potential nutrient insufficiencies that can come with eating highly processed foods and relying solely on supplements to make up the shortfall.
The variety of nutrient-dense foods available across food groups makes it easy to enjoy a satisfying, diverse, and plant-forward (though not solely plant-based) way of eating. Many of these foods provide additional health benefits including antioxidants (which are anti-inflammatory), insoluble fiber for gut health, which in turn supports overall health and wellness. Because whole foods are often more accessible and affordable than supplements, a food-based approach creates a sustainable foundation for long-term well-being.
Nutrivore encourages filling your plate with a wide range of nutrient-rich foods without the need for restrictive rules, making it easy to prevent and support health conditions through the simple power of food. With a Nutrivore approach (maximizing nutrient density across food groups), a nutritious, balanced, and enjoyable way of eating becomes both achievable and flexible for any lifestyle. While it isn’t a replacement for medical care or the advice of a registered dietitian, a balanced, food-first approach can complement your overall strategy for improving many health conditions and support long-term health goals.