Key Takeaways (expand)
- Rather than being a true vitamin, vitamin D is actually a group of fat-soluble steroid hormones—the most important for human health being vitamin D3, or cholecalciferol, and vitamin D2, or ergocalciferol.
- The liver and kidney are needed to turn vitamin D3 and vitamin D2 into the active form, 1α,25-dihydroxyvitamin D (usually shortened to 1,25(OH)2D).
- Vitamin D can be synthesized from sun exposure, with the help of a special sterol in the skin that reacts with the sun’s UVB radiation.
- The vitamin D receptor is found on nearly every cell in the body, allowing vitamin D to control the expression of over 200 genes (as well as the proteins regulated by those genes)!
- Vitamin D helps facilitate the absorption of several other minerals—namely calcium, magnesium, and phosphorus. This contributes to its role in maintaining healthy bones.
- Vitamin D is also extremely important for immunity, since most immune cells express the vitamin D receptor.
- Vitamin D plays a major role in gut health: it reduces intestinal inflammation, regulates gut barrier function, reduces the risk of inflammatory bowel diseases, and even improves the gut microbiome (reducing levels of opportunistic pathogens and increasing bacterial richness).
- Vitamin D may influence cancer risk and progression, both through its role in cellular differentiation and through direct action on cancer cells that express the vitamin D receptor. In fact, many studies have linked vitamin D with a lower risk of breast cancer and colorectal cancer!
- There’s a complex relationship between vitamin D and skin cancer, due to sun exposure increasing both vitamin D levels (which lowers cancer risk) and DNA damage in the skin (which raises cancer risk).
- Due to its effects on inflammation and immune responses, vitamin D is linked with lower risk of many autoimmune diseases—including rheumatoid arthritis, lupus, type 1 diabetes, and multiple sclerosis.
- Vitamin D contributes to cardiometabolic health through its beneficial effects on blood pressure, endothelial function, insulin sensitivity, glucose tolerance, lipid storage, fat cell formation, and hormone regulation—giving it a protective role against diabetes, cardiovascular disease, and obesity.
- Vitamin D may even boost neurological health, reducing cognitive degeneration and protecting against some neurodegenerative diseases (like Alzheimer’s and Parkinson’s disease).
- Vitamin D deficiency and insufficiency is widespread, and can lead to impaired immune function, increased risk of fractures, pregnancy complications (such as preeclampsia and gestational diabetes), rickets in children, and higher total mortality. It can also increase the risk of numerous chronic diseases.
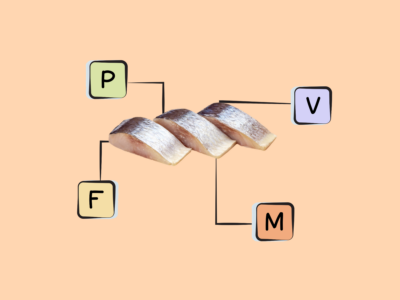
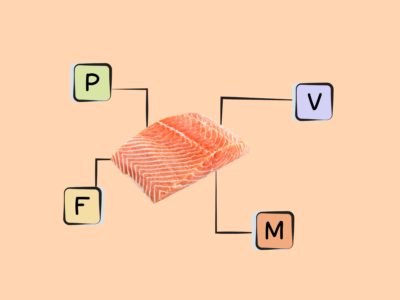
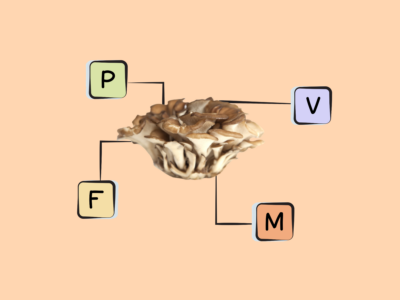
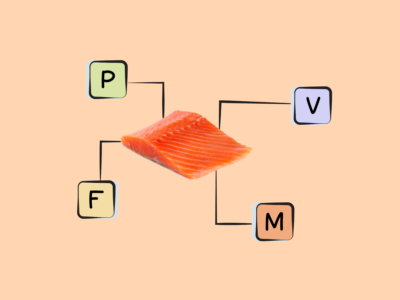
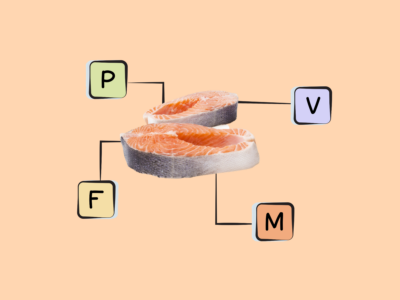
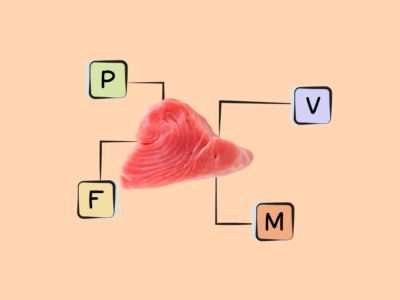
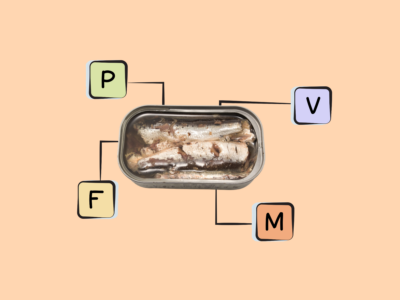
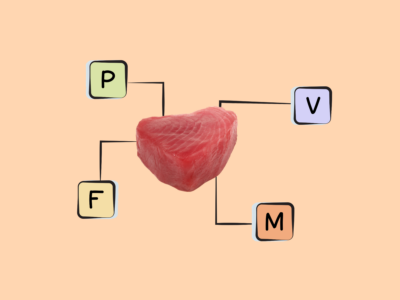
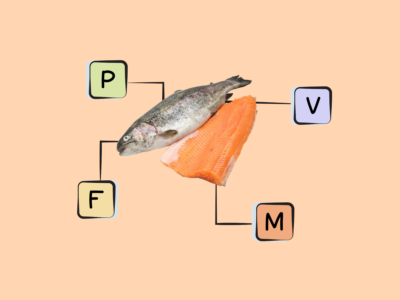
- Along with (responsible!) sunlight exposure, great sources of vitamin D include fatty fish (like salmon, sardines, herring, and mackerel), fish eggs (AKA fish roe), red meat, liver, egg yolks, and mushrooms grown under UV light.
Table of Contents[Hide][Show]
How Does Vitamin D affect Health and Disease?+−
- Vitamin D and Bone Health
- Vitamin D and Cancer
- Vitamin D and Autoimmune Disease
- Vitamin D and Cardiovascular Disease
- Vitamin D and Type 2 Diabetes
- Vitamin D and Neurodegenerative Disease
- Vitamin D and Pregnancy
- Vitamin D and Gut Health
- Vitamin D and Skin Health
- Vitamin D and Obesity
- Vitamin D and All-Cause Mortality
- what are the Health Effects of Vitamin D Deficiency?
- what are the Problems from Too Much Vitamin D?
- How Much Vitamin D Do We Need?
- what are the Best Food Sources of Vitamin D?
- What are the Good Food Sources of Vitamin D?
Despite its name, vitamin D is actually a group of fat-soluble steroid hormones rather than a true vitamin (since vitamins are defined as nutrients that must be obtained from food and can’t be synthesized by the body, which isn’t the case for vitamin D!). In humans, the most important forms are vitamin D3 (also called cholecalciferol) and vitamin D2 (also called ergocalciferol).
Fascinatingly, vitamin D is believed to be the oldest hormone on earth—having existed for at least 750 million years, when phytoplankton in the ocean began producing it in reaction to sunlight exposure. Although we don’t know exactly why it first developed, it’s likely that vitamin D helped in the evolutionary transition from water to land by allowing organisms to utilize calcium and develop skeletons.
As with some other vitamins (like vitamin A, vitamin B1, and vitamin C), the discovery of vitamin D ultimately came about from trying to cure its deficiency disease! Medical writings from the early Romans and Greeks describe the bone condition we now call rickets (caused by vitamin D deficiency), and when the Industrial Revolution arrived, rickets became more and more widespread due to dietary changes and people spending increasingly less time outdoors. For centuries, physicians tried to find a cure for this mysterious disease, with attempts ranging from painful failures (such as cauterizing veins) to successes (prescribing cod liver oil). Vitamin D was finally identified as the “fourth vitamin” in 1919, and named vitamin D a few years later (owing to the custom of naming vitamins in alphabetical order, with vitamin D following C). It took many more decades before scientists began understanding its metabolism and role in maintaining calcium and phosphate levels.
Vitamin D is important for the intestinal uptake of several other nutrients (including calcium, magnesium, and phosphorus); it’s also essential for cellular differentiation, bone density, immune function, endocrine health, and cardiovascular health.
Food sources of vitamin D include fatty fish (like salmon, mackerel, sardines, and herring), fish eggs (roe), liver, red meat, and egg yolks. Mushrooms grown under UV exposure are the only substantial non-animal-food source of naturally occurring vitamin D (mostly in the form of vitamin D2); grown under the same conditions, baker’s yeast can also produce vitamin D2. And, in some countries (including the US), a number of foods that don’t naturally contain vitamin D are fortified with it, such as store-bought orange juice, cereals, some dairy products, and plant-based milks.
Everything You Need to Jump into Nutrivore TODAY!
Nutrivore Quickstart Guide
The Nutrivore Quickstart Guide e-book explains why and how to eat a Nutrivore diet, introduces the Nutrivore Score, gives a comprehensive tour of the full range of essential and important nutrients!
Plus, you’ll find the Top 100 Nutrivore Score Foods, analysis of food groups, practical tips to increase the nutrient density of your diet, and look-up tables for the Nutrivore Score of over 700 foods.
Buy now for instant digital access.
what are The Biological Roles of Vitamin D?
One of the most unique features of vitamin D—and the reason it isn’t a true vitamin—is that our bodies can synthesize it in reaction to sun exposure. (For this reason, vitamin D is sometimes nicknamed “the sunshine vitamin”!) The skin contains a special sterol (7-dehydrocholesterol) that reacts with ultraviolet B (UVB) radiation from the sun, in turn forming vitamin D3 (cholecalciferol). Cholecalciferol then travels to the liver via the vitamin D-binding protein, where it’s further modified (into 25-hydroxyvitamin D), and then to the kidneys, where it’s activated into 1α,25-dihydroxyvitamin D (usually shortened to 1,25(OH)2D). From there, 1,25(OH)2D can bind to the vitamin D receptor (found on nearly every cell in the body), controlling the expression of more than 200 genes and the proteins that those genes regulate! After reaching circulation, dietary vitamin D3 and D2 undergo the same processes as vitamin D produced from sunlight.
Vitamin D is also crucial for regulating several key components of the immune system. For example, it modulates immunity by acting through the vitamin D receptor, which is expressed by most immune cells (including dendritic cells, macrophages, and regulatory T cells). Under some circumstances, immune cells can also express an enzyme to produce 1,25(OH)2D themselves, which then acts to regulate the local immune response.
Research has shown that vitamin D helps regulate gastrointestinal inflammation and enhances gut barrier function. Vitamin D also activates proteins important for detoxifying lithocholic acid (a secondary bile acid that’s toxic for intestinal cells). One way vitamin D helps maintain the integrity of the gut mucosal barrier is by enhancing the intercellular junctions that control gut permeability, as well as reducing inflammatory cytokines like interleukin-8.
Additional roles of vitamin D include the biosynthesis of neurotrophic factors, regulating the release of important hormones like serotonin and insulin. For example, insulin-secreting cells in the pancreas express the vitamin D receptor, and vitamin D plays a role in insulin secretion during conditions where insulin demands are higher. And, vitamin D is involved in blood pressure regulation (through its influence on the renin-angiotensin system), as well as wound healing (through its role in cell growth).
How Does Vitamin D Interact with Other Nutrients?
Vitamin D is also famously important for mineral metabolism: it regulates the absorption and transport of calcium, phosphorous, and magnesium.
Calcium balance is particularly important to maintain, because any alterations outside a very narrow range in the blood can negatively impact nervous system functioning and bone health. Here, vitamin D works with the parathyroid gland to determine how much calcium will be deposited or removed from bones, as well as by modifying the amount of calcium that’s excreted by the kidneys and how much is absorbed in the gut during digestion. When the parathyroid gland detects that blood calcium levels are dropping too low, it secretes parathyroid hormone, which in turn stimulates the activity of an enzyme in the kidney (called 25-hydroxyvitamin D3-1α-hydroxylase) that increases the production of the active form of vitamin D (1,25(OH)2D). This active vitamin D is then released into circulation, travels to target tissues, and induces the activation of the vitamin D receptor—in turn altering the expression of genes that normalize calcium levels through various mechanisms. As a result of this process, calcium levels can be kept within the range needed for the body’s vital functions, all with the help of vitamin D!
Phosphorus balance, too, is dependent on vitamin D; in fact, phosphorus metabolism operates in parallel to calcium metabolism. Both parathyroid hormone and 1,25(OH)2D help control blood levels of phosphorus, such as by increasing phosphorus absorption in the small intestine and by directing the kidneys to reduce how much phosphorus is resorbed (leading to increased urinary excretion).
Want to know the top 25 foods for this awesome nutrient?

The Top 25 Foods for Every Nutrient
The Top 25 Foods for Every Nutrient e-book is a well-organized, easy-to-use, grocery store-friendly guide to help you choose foods that fit your needs of 43 important nutrients while creating a balanced nutrient-dense diet.
Get two “Top 25” food lists for each nutrient, plus you’ll find RDA charts for everyone, informative visuals, fun facts, serving sizes and the 58 foods that are Nutrient Super Stars!
Buy now for instant digital access.
How Does Vitamin D affect Health and Disease?
Vitamin D is important for the intestinal uptake of several other nutrients (including calcium, magnesium, and phosphorus); it’s also essential for cellular differentiation, bone density, immune function, endocrine health, and cardiovascular health.
Vitamin D and Bone Health
Because of its role in regulating calcium and phosphorus levels (two key components of bone), vitamin D is essential for healthy bones. In elderly adults with osteoporosis, low vitamin D status is disproportionately common, and clinical trials have shown that supplementing with 800 international units (IU) daily of vitamin D can reduce the risk of bone fractures and falls. Prospective cohort studies have also shown that people consuming at least 600 IU of vitamin D daily have over a third lower risk of developing osteoporotic hip fractures compared to people consuming under 140 IU per day. And, multiple meta-analyses have shown that vitamin D supplementation (with or without calcium) leads to a significantly lower risk of fractures, including both hip fractures and any non-spine fractures. On the whole, vitamin D is truly vital for strong bones!
Vitamin D and Cancer
Vitamin D also has some compelling links with cancer risk, due in part to its role in regulating cell differentiation (where cells become specialized for specific functions) and to its effects on cancer cells that express the vitamin D receptor (mechanistic studies show that when active vitamin D binds to the vitamin D receptor, it can control the fate of cancer cells by inhibiting their proliferation or inducing their death!). Observational research shows fairly consistent associations between low sunlight exposure, low vitamin D levels, and greater risk of breast cancer and colorectal cancer (in fact, the geographical distribution of rickets and modern colon cancer mortality are very similar). And, for each 20 ng/mL increase in circulating vitamin D levels, prospective studies have found that cancer incidence drops by 11% and cancer death drops by 17%. Interestingly, some studies have found that the protective effect of vitamin D on cancer is stronger in women than in men.
Studies of specific cancer types show that there’s up to a 38% lower risk of developing colon cancer among people with the highest versus lowest circulating vitamin D levels, and for patients who already have colorectal cancer, an estimated 10% lower risk of dying from it for every 8 ng/mL increase in serum vitamin D. (However, we need more controlled studies to examine the effects of vitamin D interventions on colorectal risk and outcomes.)
Some prospective research also shows that women who get adequate vitamin D intake and sun exposure have a significantly lower risk of developing breast cancer over the course of the next two decades, and that patients with early-stage breast cancer have a better prognosis when their vitamin D status is adequate. But, meta-analyses have turned up inconsistent results when multiple observational studies are pooled together, with some showing a protective effect of vitamin D, some showing no relationship, and some showing significance only among certain subgroups (such as postmenopausal but not premenopausal women).
Some emerging (but still limited!) evidence also shows a potential relationship between vitamin D and reduced risk of lung cancer and bladder cancer.
When it comes to skin cancer, the role of vitamin D is complex. On one hand, some observational research has linked higher vitamin D status to an increased risk of certain skin cancers, including squamous cell carcinoma and basal cell carcinoma—likely due to vitamin D status correlating with sun exposure, which is known to increase skin cancer risk (due to damaging the DNA in skin cells). However, vitamin D appears to boost survival for people already diagnosed with skin cancer, especially malignant melanoma. Studies show that higher vitamin D status at the time of diagnosis is associated with a better prognosis for melanoma patients, whereas vitamin D deficiency at the time of diagnosis is associated with lower survival and more aggressive progression of the disease. So, staying vitamin D-replete without excessive levels of sun exposure appears important for harnessing the anti-cancer effects of vitamin D without inadvertently increasing skin cancer risk.
Vitamin D and Autoimmune Disease
Another health benefit of vitamin D is its potential for protecting against a number of autoimmune diseases—including type 1 diabetes, rheumatoid arthritis, multiple sclerosis, and lupus. This is due to vitamin D’s ability to decrease inflammation and mediate the activity of T cells, which in turn modulate autoimmune responses; genetic variations that affect vitamin D metabolism may also mediate its protective effects.
In some cases, vitamin D status very early in life or even in utero could influence the risk of developing autoimmune conditions later on; for example, one study found that children given vitamin D supplements during their first year of life had an 88% lower risk of developing type 1 diabetes over the course of the next 30 years, and also found a significant relationship between rickets during infancy and the subsequent development of type 1 diabetes. And, another study showed when mothers have low vitamin D levels during pregnancy (especially the third trimester), the risk of their offspring developing type 1 diabetes appears to be over twice as high compared to when maternal vitamin D status is adequate. Similarly, maternal sun exposure (as a potential proxy for vitamin D) has shown an inverse relationship with multiple sclerosis incidence among their offspring, while sunscreen use and infrequent outdoor activities in early childhood leads to an increased risk later in life.
In adults, too, higher vitamin D status and use of vitamin D supplements (at least 400 IU daily) have both been associated with reduced incidence of multiple sclerosis, and among patients who do have the disease, vitamin D status appears predictive of its severity and progression over time. Rheumatoid arthritis also has a potential link to vitamin D, with variations in the gene coding for the vitamin D receptor apparently influencing rheumatoid arthritis risk, and some observational research showing that people with the highest (versus lowest) vitamin D intakes have a 33% lower risk of developing rheumatoid arthritis. And while the results of clinical trials have been mixed, some evidence suggests that supplementing with vitamin D can improve the symptom severity, disease activity, and inflammatory markers of another autoimmune condition, systemic lupus erythematosus. (Lupus patients may be particularly susceptible to vitamin D insufficiency because sunlight is known to aggravate symptoms!)
Vitamin D and Cardiovascular Disease
Some components of cardiovascular health are also linked to vitamin D status. For example, due to its role in inhibiting renin synthesis (as part of the renin-angiotensis system), vitamin D can help lower blood pressure; some studies suggest a 12% lower risk of hypertension for every 10 ng/mL increase in serum vitamin D levels. And endothelial function, another contributor to cardiovascular health, is responsive to vitamin D—with research showing a positive correlation between serum vitamin D and flow-mediated dilation (a marker of vascular health), and trials demonstrating that high-dose vitamin D supplementation can reduce endothelial dysfunction markers.
Prospective studies have also shown that low vitamin D status is associated with a higher incidence of stroke, heart failure, and coronary artery disease. However, clinical trials haven’t shown a clear benefit of vitamin D supplementation on actual cardiac events, so more research here is needed!
Vitamin D and Type 2 Diabetes
For people already at high risk for type 2 diabetes, every 4 ng/mL increase of serum vitamin D is estimated to reduce progression to diabetes by 23%!
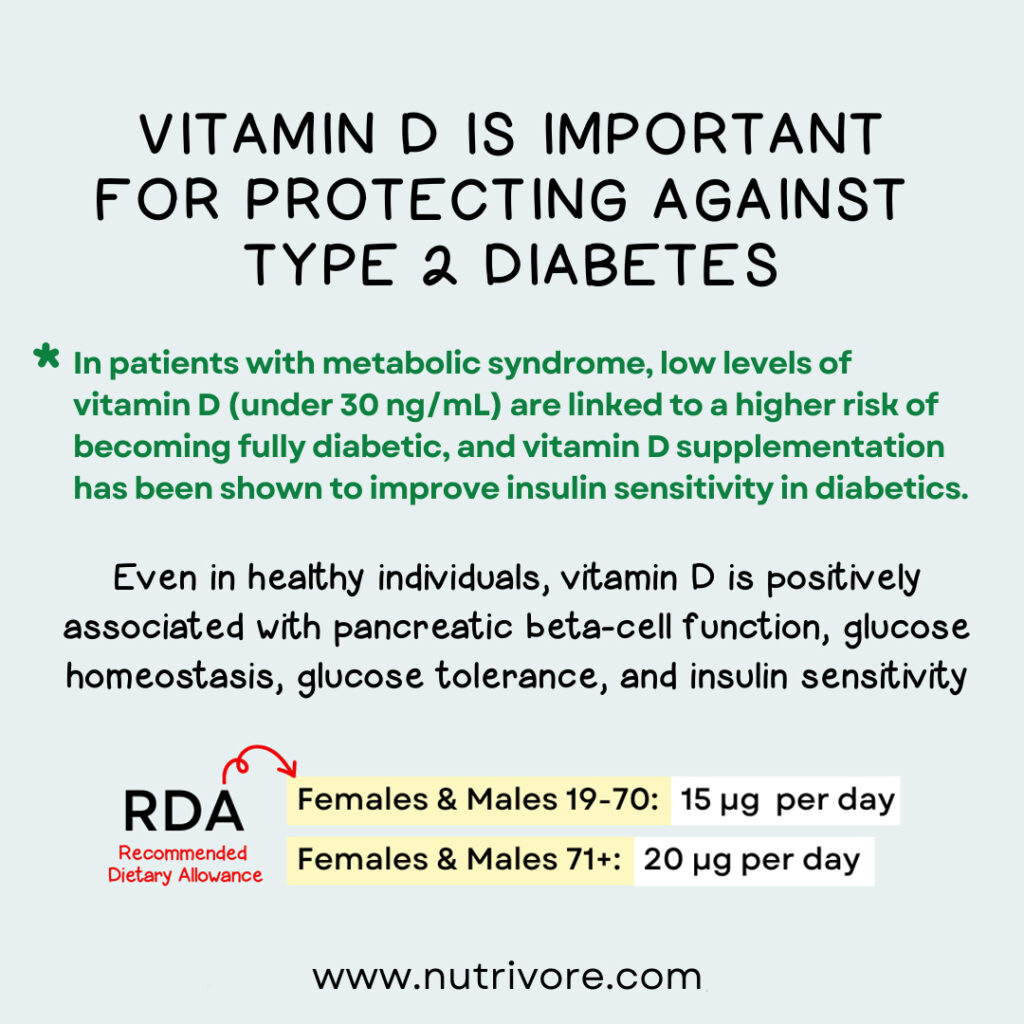
Vitamin D is also important for protecting against type 2 diabetes. In patients with metabolic syndrome, low levels of vitamin D (under 30 ng/mL) are linked to a higher risk of becoming fully diabetic, and vitamin D supplementation has been shown to improve insulin sensitivity in diabetics. Even in healthy individuals, vitamin D is positively associated with pancreatic beta-cell function, insulin sensitivity, glucose homeostasis, glucose tolerance, and insulin sensitivity. And, across a spectrum of prospective studies, people with the highest (versus lowest) circulating vitamin D levels and/or vitamin D intakes have shown a consistently reduced risk of developing type 2 diabetes over the span of many years. For people already at high risk of the disease, every 4 ng/mL increase of serum vitamin D is estimated to reduce progression to diabetes by 23%!
Vitamin D and Neurodegenerative Disease
Some evidence suggests that vitamin D could help reduce cognitive deterioration in some neurodegenerative diseases. Experimental studies show that insufficient vitamin D may play a role in neuron degeneration and the loss of cognitive function, due to vitamin D’s role in regulating calcium channels, neuroprotection, and immunomodulation within the central nervous system.
Some (though not all) observational studies have shown a protective link between vitamin D status and/or dietary vitamin D and mild cognitive impairment, the development of Alzheimer’s disease, and specific cognitive deficits involving semantic memory, retrograde episodic memory, and orientation in time.
In patients with Parkinson’s disease, vitamin D supplementation has been shown to limit the progression of the disease (compared to a placebo group), and low vitamin D in general has been associated with a greater likelihood of developing Parkinson’s among people who are initially healthy.
Vitamin D and Pregnancy
During pregnancy, getting enough vitamin D is particularly important for preventing adverse outcomes. Low vitamin D is associated with a greater risk of preeclampsia, bacterial vaginosis, and gestational diabetes, as well as higher odds of delivering low-birth-weight infants. But, there isn’t enough evidence yet to show how vitamin D supplementation affects these outcomes.
Vitamin D and Gut Health
Vitamin D is also important for maintaining gut health. Observational studies have shown that people with higher levels of vitamin D are less likely to develop inflammatory bowel diseases, especially Crohn’s disease and ulcerative colitis; higher vitamin D status is also associated with less severe disease among people who already have these conditions. Vitamin D supplementation has likewise been shown to reduce the relapse rate in Crohn’s disease patients in remission. Vitamin D’s benefit here may be due to its ability to reduce intestinal inflammation.
Meanwhile, the composition of the gut microbiome is sensitive to our vitamin D status. Several studies have found that vitamin D supplementation significantly reduces levels of some most common opportunistic pathogens, while also increasing the bacterial richness of the gut microbiome (a signature feature of gut health!). And, people with higher levels of vitamin D have been shown to have lower levels of harmful endotoxin in the blood, possibly due to vitamin D’s ability to improve gut barrier integrity.
The THREE Best Probiotics
Bacillus/Spore-based

Best for a general probiotic, if you were recently on antibiotics, or for digestion issues (especially abdominal pain, bloating, flatulence, diarrhea, and gas after meals).
Lactobacillus & Bifidobacterium

Best for if you don’t eat fermented foods, if you were recently on antibiotics, or if you have issues with constipation or gas.
Saccharomyces boulardii

Best for if you have Candida issues, were recently on antibiotics, or have diarrhea.
Vitamin D and Skin Health
Additionally, vitamin D may help with eczema, also known as atopic dermatitis. In multiple controlled studies, daily vitamin D supplementation was able to significantly reduce the intensity and extent of patients’ eczema—possibly through stimulating microbial activities in the skin, or through regulating local inflammatory reactions.
Vitamin D and Obesity
There’s also some evidence linking vitamin D with body weight and obesity. Several double-blind clinical trials found that supplementing with vitamin D for six to 12 weeks led to significant decreases in body weight, waist circumference, body mass index, and fat mass. And, observational research has linked higher vitamin D levels to less weight gain over time.
Although the possible mechanisms behind this relationship require more study, some evidence suggests that vitamin D could help reduce the formation of fat cells, as well as decrease lipid storage within fat cells.
Vitamin D and All-Cause Mortality
Vitamin D has also been linked with total mortality. Across a variety of observational studies, the risk of all-cause mortality has been shown to increase as vitamin D levels decline (particularly when serum levels are under 16 ng/mL), or when people with the lowest serum vitamin D concentrations are compared to people with the highest.
Didn’t know vitamin D was this amazing? Maybe your friends will enjoy this too!
what are the Health Effects of Vitamin D Deficiency?
Vitamin D is one of the most common nutrient deficiencies, particularly in industrialized countries where people spend more time indoors (and therefore get limited sun exposure). In fact, about 75% of Westerners are deficient in vitamin D.
Over time, vitamin D deficiency may contribute to a wide range of chronic diseases.
A number of factors can increase the risk of vitamin D deficiency, including:
- environmental conditions (living in cloudy climates or at high latitudes),
- reduced skin exposure to the sun (such as from a concealed clothing style for religious or cultural reasons, or always wearing sunscreen and protective clothing to avoid sun damage),
- skin pigmentation (people with dark skin produce less vitamin D from sun exposure),
- genetic variations (certain common gene variations involved in cholesterol synthesis, vitamin D transport, and hydroxylation have been shown to influence vitamin D status),
- inflammatory bowel diseases or fat malabsorption syndromes (which reduce dietary vitamin D uptake or hinder its conversion into the active form),
- having cystic fibrosis (which impairs the absorption and metabolism of fat-soluble vitamins),
- older age (elderly individuals have a lower capacity to synthesize vitamin D,
- obesity (due to vitamin D being sequestered in body fat stores and reducing its bioavailability), or
- magnesium deficiency (due to magnesium regulating the activity of some enzymes involved in vitamin D metabolism).
Due to the importance of the liver and kidney in converting inactive vitamin D into its active form, people with liver or kidney disease are also more likely to experience low vitamin D levels.
In children, severe vitamin D causes rickets—a condition where rapidly-growing bones don’t properly mineralize, leading to a bowed shape in the arms and legs, rib cage deformities, delayed closure of the soft spots in infant skulls, and in some cases (when a lack of vitamin D prevents calcium levels from properly regulating), seizures. In adults, vitamin D deficiency leads to osteomalacia—a progressive loss of bone mineral that leads to a softening of the bone tissue, bone pain, and a greater risk of developing osteoporosis.
Other symptoms of vitamin D deficiency include muscle weakness and pain, fatigue, mood changes like depression, and secondary hyperparathyroidism, which increases the breakdown of bone and ultimately lead to osteoporosis. Over time, vitamin D deficiency may contribute to a wide range of chronic diseases.
Nutrivore Is a Game-Changer—This FREE Guide Shows You Why
Sign up for the free Nutrivore Newsletter, your weekly, science-backed guide to improving health through nutrient-rich foods — without dieting harder —and get the Beginner’s Guide to Nutrivore delivered straight to your inbox!

what are the Problems from Too Much Vitamin D?
With vitamin D, as with many nutrients, it’s possible to get too much of a good thing. While vitamin D toxicity hasn’t been demonstrated from sun exposure alone, and is very unlikely to happen even at intakes of up to 10,000 IU per day, it can potentially occur from extremely high-dose dietary supplements (especially upwards of 50,000 IU daily), leading to hypercalcemia (elevated calcium levels in the blood). This can then result in kidney stones, bone loss, and heart or kidney calcification, along with symptoms such as fatigue, constipation, muscle weakness, vomiting, diarrhea, irritability, and dehydration. Some people may be at higher risk of vitamin D-induced hypercalcemia, particularly people with sarcoidosis, tuberculosis, lymphoma, and hyperparathyroidism.
So, if you’re considering supplementing with high doses of vitamin D, be sure to seek medical advice from a health care professional to avoid potential harm!
How Much Vitamin D Do We Need?
Because vitamin D can come from both food and our body’s own synthesis, it’s been difficult to establish a guidelines for the amount of vitamin D each individual needs. The current recommended dietary allowance (RDA) is 600 IU per day for adults (800 IU per day after the age of 70), with a tolerable upper limit set at 4000 IU daily (meaning beyond this level, the risk of harm begins to increase). However, for those with vitamin D deficiency or insufficiency, many medical professionals are shifting towards individualized doses of vitamin D supplements to sustain optimal serum levels, rather than a standard supplementation dose. This involves testing 25-hydroxyvitamin D level every 3 to 6 months, and adjusting the dose of vitamin D supplementation accordingly.
Some research suggests that higher vitamin D intakes may be necessary while breastfeeding in order to produce milk with high enough vitamin D content to meet the infants’ needs. In these cases, breastfeeding individuals may need to supplement with additional vitamin D—possibly as much as 4000 to 4600 IU daily, or a monthly dose of 150,000 IU. Alternatively, the American Academy of Pediatrics recommends that breastfed infants receive 400 IU of supplemental vitamin D each day in addition to breast milk.
It’s important to note that we can store vitamin D in the liver (during the winter months, for example), so intakes can fluctuate without immediately causing a deficiency. However, these recommended intakes don’t account for the many factors that influence vitamin D status as a whole, particularly sun exposure, and having darker skin. What’s important is that blood levels remain in the optimal range—whether that’s achieved through diet, supplementation, or time in the sunshine!
Scientists generally agree that the best indicator of vitamin D status is the serum 25-hydroxyvitamin D concentration, with optimum levels being between 50 and 70 ng/mL (deficiency is considered 20 ng/mL and below, and insufficiency is considered below 30 ng/mL).
| 0 – 6 months | |||||
| 6 months to < 12 months | |||||
| 1 yr – 3 yrs | |||||
| 4 yrs – 8 yrs | |||||
| 9 yrs – 13 yrs | |||||
| 14 yrs – 18 yrs | |||||
| 19 yrs – 50 yrs | |||||
| 51+ yrs | |||||
| Pregnant (14 – 18 yrs) | |||||
| Pregnant (19 – 30 yrs) | |||||
| Pregnant (31 – 50 yrs) | |||||
| Lactating (14 – 18 yrs) | |||||
| Lactating (19 – 30 yrs) | |||||
| Lactating (31 – 50 yrs) |
Nutrient Daily Values
Nutrition requirements and recommended nutrient intake for infants, children, adolescents, adults, mature adults, and pregnant and lactating individuals.
what are the Best Food Sources of Vitamin D?
The following foods have high concentrations of vitamin D, containing at least 50% of the recommended dietary allowance per serving, making them our best food sources of this valuable vitamin steroid hormone!
Want to know the top 500 most nutrient-dense foods?

Top 500 Nutrivore Foods
The Top 500 Nutrivore Foods e-book is an amazing reference deck of the top 500 most nutrient-dense foods according to their Nutrivore Score. Think of it as the go-to resource for a super-nerd, to learn more and better understand which foods stand out, and why!
If you are looking for a quick-reference guide to help enhance your diet with nutrients, and dive into the details of your favorite foods, this book is your one-stop-shop!
Buy now for instant digital access.
What are the Good Food Sources of Vitamin D?
The following foods are also excellent or good sources of vitamin D, containing at least 10% (and up to 50%) of the daily value per serving.

Merch and Household Goods
Check out our collection of practical and nerdtastic T-shirts, totes, and more!
Citations
Expand to see all scientific references for this article.
Ahn J, Yu K, Stolzenberg-Solomon R, Simon KC, McCullough ML, Gallicchio L, Jacobs EJ, Ascherio A, Helzlsouer K, Jacobs KB, Li Q, Weinstein SJ, Purdue M, Virtamo J, Horst R, Wheeler W, Chanock S, Hunter DJ, Hayes RB, Kraft P, Albanes D. Genome-wide association study of circulating vitamin D levels. Hum Mol Genet. 2010 Jul 1;19(13):2739-45. doi: 10.1093/hmg/ddq155.
Al Mheid I, Patel R, Murrow J, Morris A, Rahman A, Fike L, Kavtaradze N, Uphoff I, Hooper C, Tangpricha V, Alexander RW, Brigham K, Quyyumi AA. Vitamin D status is associated with arterial stiffness and vascular dysfunction in healthy humans. J Am Coll Cardiol. 2011 Jul 5;58(2):186-92. doi: 10.1016/j.jacc.2011.02.051.
Al-Khalidi B, Kimball SM, Rotondi MA, Ardern CI. Standardized serum 25-hydroxyvitamin D concentrations are inversely associated with cardiometabolic disease in U.S. adults: a cross-sectional analysis of NHANES, 2001-2010. Nutr J. 2017 Feb 28;16(1):16. doi: 10.1186/s12937-017-0237-6.
Ananthakrishnan AN, Khalili H, Higuchi LM, Bao Y, Korzenik JR, Giovannucci EL, Richter JM, Fuchs CS, Chan AT. Higher predicted vitamin D status is associated with reduced risk of Crohn’s disease. Gastroenterology. 2012 Mar;142(3):482-9. doi: 10.1053/j.gastro.2011.11.040.
Annweiler C, Fantino B, Schott AM, Krolak-Salmon P, Allali G, Beauchet O. Vitamin D insufficiency and mild cognitive impairment: cross-sectional association. Eur J Neurol. 2012 Jul;19(7):1023-9. doi: 10.1111/j.1468-1331.2012.03675.x.
Annweiler C, Milea D, Whitson HE, Cheng CY, Wong TY, Ikram MK, Lamoureux EL, Sabanayagam C. Vitamin D insufficiency and cognitive impairment in Asians: a multi-ethnic population-based study and meta-analysis. J Intern Med. 2016 Sep;280(3):300-11. doi: 10.1111/joim.12491.
Annweiler C, Rolland Y, Schott AM, Blain H, Vellas B, Herrmann FR, Beauchet O. Higher vitamin D dietary intake is associated with lower risk of alzheimer’s disease: a 7-year follow-up. J Gerontol A Biol Sci Med Sci. 2012 Nov;67(11):1205-11. doi: 10.1093/gerona/gls107.
Antico A, Tampoia M, Tozzoli R, Bizzaro N. Can supplementation with vitamin D reduce the risk or modify the course of autoimmune diseases? A systematic review of the literature. Autoimmun Rev. 2012 Dec;12(2):127-36. doi: 10.1016/j.autrev.2012.07.007.
Aranow C. Vitamin D and the immune system. J Investig Med. 2011 Aug;59(6):881-6. doi: 10.2310/JIM.0b013e31821b8755.
Balion C, Griffith LE, Strifler L, Henderson M, Patterson C, Heckman G, Llewellyn DJ, Raina P. Vitamin D, cognition, and dementia: a systematic review and meta-analysis. Neurology. 2012 Sep 25;79(13):1397-405. doi: 10.1212/WNL.0b013e31826c197f.
Bashir M, Prietl B, Tauschmann M, Mautner SI, Kump PK, Treiber G, Wurm P, Gorkiewicz G, Högenauer C, Pieber TR. Effects of high doses of vitamin D3 on mucosa-associated gut microbiome vary between regions of the human gastrointestinal tract. Eur J Nutr. 2016 Jun;55(4):1479-89. doi: 10.1007/s00394-015-0966-2.
Bassil D, Rahme M, Hoteit M, Fuleihan Gel-H. Hypovitaminosis D in the Middle East and North Africa: Prevalence, risk factors and impact on outcomes. Dermatoendocrinol. 2013 Apr 1;5(2):274-98. doi: 10.4161/derm.25111.
Bikle DD. Vitamin D metabolism, mechanism of action, and clinical applications. Chem Biol. 2014 Mar 20;21(3):319-29. doi: 10.1016/j.chembiol.2013.12.016.
Bikle DD. Vitamin D: an ancient hormone. Exp Dermatol. 2011 Jan;20(1):7-13. doi: 10.1111/j.1600-0625.2010.01202.x. PMID: 21197695.
Bjelakovic G, Gluud LL, Nikolova D, Whitfield K, Wetterslev J, Simonetti RG, Bjelakovic M, Gluud C. Vitamin D supplementation for prevention of mortality in adults. Cochrane Database Syst Rev. 2014 Jan 10;(1):CD007470. doi: 10.1002/14651858.CD007470.pub3.
Cardwell G, Bornman JF, James AP, Black LJ. A Review of Mushrooms as a Potential Source of Dietary Vitamin D. Nutrients. 2018 Oct 13;10(10):1498. doi: 10.3390/nu10101498.
Chapuy MC, Preziosi P, Maamer M, Arnaud S, Galan P, Hercberg S, Meunier PJ. Prevalence of vitamin D insufficiency in an adult normal population. Osteoporos Int. 1997;7(5):439-43. doi: 10.1007/s001980050030.
Chiu KC, Chu A, Go VL, Saad MF. Hypovitaminosis D is associated with insulin resistance and beta cell dysfunction. Am J Clin Nutr. 2004 May;79(5):820-5. doi: 10.1093/ajcn/79.5.820.
Choi YJ, Kim YH, Cho CH, Kim SH, Lee JE. Circulating levels of vitamin D and colorectal adenoma: A case-control study and a meta-analysis. World J Gastroenterol. 2015 Aug 7;21(29):8868-77. doi: 10.3748/wjg.v21.i29.8868.
Chowdhury R, Kunutsor S, Vitezova A, Oliver-Williams C, Chowdhury S, Kiefte-de-Jong JC, Khan H, Baena CP, Prabhakaran D, Hoshen MB, Feldman BS, Pan A, Johnson L, Crowe F, Hu FB, Franco OH. Vitamin D and risk of cause specific death: systematic review and meta-analysis of observational cohort and randomised intervention studies. BMJ. 2014 Apr 1;348:g1903. doi: 10.1136/bmj.g1903.
Chung M, Lee J, Terasawa T, Lau J, Trikalinos TA. Vitamin D with or without calcium supplementation for prevention of cancer and fractures: an updated meta-analysis for the U.S. Preventive Services Task Force. Ann Intern Med. 2011 Dec 20;155(12):827-38. doi: 10.7326/0003-4819-155-12-201112200-00005. Erratum in: Ann Intern Med. 2014 Oct 21;161(8):615-6.
Deng X, Song Y, Manson JE, Signorello LB, Zhang SM, Shrubsole MJ, Ness RM, Seidner DL, Dai Q. Magnesium, vitamin D status and mortality: results from US National Health and Nutrition Examination Survey (NHANES) 2001 to 2006 and NHANES III. BMC Med. 2013 Aug 27;11:187. doi: 10.1186/1741-7015-11-187.
Ekmekcioglu C, Haluza D, Kundi M. 25-Hydroxyvitamin D Status and Risk for Colorectal Cancer and Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis of Epidemiological Studies. Int J Environ Res Public Health. 2017 Jan 28;14(2):127. doi: 10.3390/ijerph14020127.
Gallagher JC, Yalamanchili V, Smith LM. The effect of vitamin D supplementation on serum 25(OH)D in thin and obese women. J Steroid Biochem Mol Biol. 2013 Jul;136:195-200. doi: 10.1016/j.jsbmb.2012.12.003.
Gandini S, Boniol M, Haukka J, Byrnes G, Cox B, Sneyd MJ, Mullie P, Autier P. Meta-analysis of observational studies of serum 25-hydroxyvitamin D levels and colorectal, breast and prostate cancer and colorectal adenoma. Int J Cancer. 2011 Mar 15;128(6):1414-24. doi: 10.1002/ijc.25439.
Garland CF, Garland FC, Gorham ED. Calcium and vitamin D. Their potential roles in colon and breast cancer prevention. Ann N Y Acad Sci. 1999;889:107-19. doi: 10.1111/j.1749-6632.1999.tb08728.x.
Gröber U, Spitz J, Reichrath J, Kisters K, Holick MF. Vitamin D: Update 2013: From rickets prophylaxis to general preventive healthcare. Dermatoendocrinol. 2013 Jun 1;5(3):331-47. doi: 10.4161/derm.26738.
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Murad MH, Weaver CM; Endocrine Society. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011 Jul;96(7):1911-30. doi: 10.1210/jc.2011-0385. Epub 2011 Jun 6. Erratum in: J Clin Endocrinol Metab. 2011 Dec;96(12):3908.
Holick MF. Vitamin D: importance in the prevention of cancers, type 1 diabetes, heart disease, and osteoporosis. Am J Clin Nutr. 2004 Mar;79(3):362-71. doi: 10.1093/ajcn/79.3.362.
Hu K, Callen DF, Li J, Zheng H. Circulating Vitamin D and Overall Survival in Breast Cancer Patients: A Dose-Response Meta-Analysis of Cohort Studies. Integr Cancer Ther. 2018 Jun;17(2):217-225. doi: 10.1177/1534735417712007.
Hyppönen E, Läärä E, Reunanen A, Järvelin MR, Virtanen SM. Intake of vitamin D and risk of type 1 diabetes: a birth-cohort study. Lancet. 2001 Nov 3;358(9292):1500-3. doi: 10.1016/S0140-6736(01)06580-1.
Jahnsen J, Falch JA, Mowinckel P, Aadland E. Vitamin D status, parathyroid hormone and bone mineral density in patients with inflammatory bowel disease. Scand J Gastroenterol. 2002 Feb;37(2):192-9. doi: 10.1080/003655202753416876.
John EM, Schwartz GG, Dreon DM, Koo J. Vitamin D and breast cancer risk: the NHANES I Epidemiologic follow-up study, 1971-1975 to 1992. National Health and Nutrition Examination Survey. Cancer Epidemiol Biomarkers Prev. 1999 May;8(5):399-406.
Jones AN, Hansen KE. Recognizing the musculoskeletal manifestations of vitamin D deficiency. J Musculoskelet Med. 2009 Oct;26(10):389-396.
Khan H, Kunutsor S, Franco OH, Chowdhury R. Vitamin D, type 2 diabetes and other metabolic outcomes: a systematic review and meta-analysis of prospective studies. Proc Nutr Soc. 2013 Feb;72(1):89-97. doi: 10.1017/S0029665112002765.
Khosravi ZS, Kafeshani M, Tavasoli P, Zadeh AH, Entezari MH. Effect of Vitamin D Supplementation on Weight Loss, Glycemic Indices, and Lipid Profile in Obese and Overweight Women: A Clinical Trial Study. Int J Prev Med. 2018 Jul 20;9:63. doi: 10.4103/ijpvm.IJPVM_329_15.
Kim G, Bae JH. Vitamin D and atopic dermatitis: A systematic review and meta-analysis. Nutrition. 2016 Sep;32(9):913-20. doi: 10.1016/j.nut.2016.01.023.
Kim Y, Je Y. Vitamin D intake, blood 25(OH)D levels, and breast cancer risk or mortality: a meta-analysis. Br J Cancer. 2014 May 27;110(11):2772-84. doi: 10.1038/bjc.2014.175.
Kunutsor SK, Apekey TA, Steur M. Vitamin D and risk of future hypertension: meta-analysis of 283,537 participants. Eur J Epidemiol. 2013 Mar;28(3):205-21. doi: 10.1007/s10654-013-9790-2.
Lacroix M, Battista MC, Doyon M, Houde G, Ménard J, Ardilouze JL, Hivert MF, Perron P. Lower vitamin D levels at first trimester are associated with higher risk of developing gestational diabetes mellitus. Acta Diabetol. 2014 Aug;51(4):609-16. doi: 10.1007/s00592-014-0564-4.
Lee YH, Bae SC. Vitamin D level in rheumatoid arthritis and its correlation with the disease activity: a meta-analysis. Clin Exp Rheumatol. 2016 Sep-Oct;34(5):827-833.
Liao Y, Huang JL, Qiu MX, Ma ZW. Impact of serum vitamin D level on risk of bladder cancer: a systemic review and meta-analysis. Tumour Biol. 2015 Mar;36(3):1567-72. doi: 10.1007/s13277-014-2728-9.
Lin J, Liu J, Davies ML, Chen W. Serum Vitamin D Level and Rheumatoid Arthritis Disease Activity: Review and Meta-Analysis. PLoS One. 2016 Jan 11;11(1):e0146351. doi: 10.1371/journal.pone.0146351.
Lin R, White JH. The pleiotropic actions of vitamin D. Bioessays. 2004 Jan;26(1):21-8. doi: 10.1002/bies.10368.
Lips P, van Schoor NM. The effect of vitamin D on bone and osteoporosis. Best Pract Res Clin Endocrinol Metab. 2011 Aug;25(4):585-91. doi: 10.1016/j.beem.2011.05.002.
Looker AC, Johnson CL, Lacher DA, Pfeiffer CM, Schleicher RL, Sempos CT. Vitamin D status: United States, 2001-2006. NCHS Data Brief. 2011 Mar;(59):1-8.
Lu M, Xu Y, Lv L, Zhang M. Association between vitamin D status and the risk of gestational diabetes mellitus: a meta-analysis. Arch Gynecol Obstet. 2016 May;293(5):959-66. doi: 10.1007/s00404-016-4010-4.
Lucato P, Solmi M, Maggi S, Bertocco A, Bano G, Trevisan C, Manzato E, Sergi G, Schofield P, Kouidrat Y, Veronese N, Stubbs B. Low vitamin D levels increase the risk of type 2 diabetes in older adults: A systematic review and meta-analysis. Maturitas. 2017 Jun;100:8-15. doi: 10.1016/j.maturitas.2017.02.016.
Lv Z, Qi H, Wang L, Fan X, Han F, Wang H, Bi S. Vitamin D status and Parkinson’s disease: a systematic review and meta-analysis. Neurol Sci. 2014 Nov;35(11):1723-30. doi: 10.1007/s10072-014-1821-6.
Ma Y, Zhang P, Wang F, Yang J, Liu Z, Qin H. Association between vitamin D and risk of colorectal cancer: a systematic review of prospective studies. J Clin Oncol. 2011 Oct 1;29(28):3775-82. doi: 10.1200/JCO.2011.35.7566.
Martineau AR, Jolliffe DA, Hooper RL, Greenberg L, Aloia JF, Bergman P, Dubnov-Raz G, Esposito S, Ganmaa D, Ginde AA, Goodall EC, Grant CC, Griffiths CJ, Janssens W, Laaksi I, Manaseki-Holland S, Mauger D, Murdoch DR, Neale R, Rees JR, Simpson S Jr, Stelmach I, Kumar GT, Urashima M, Camargo CA Jr. Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ. 2017 Feb 15;356:i6583. doi: 10.1136/bmj.i6583.
Mazidi M, Karimi E, Rezaie P, Vatanparast H. The impact of vitamin D supplement intake on vascular endothelial function; a systematic review and meta-analysis of randomized controlled trials. Food Nutr Res. 2017 Mar 20;61(1):1273574. doi: 10.1080/16546628.2016.1273574. PMID: 28469540; PMCID: PMC5404423.
Merlino LA, Curtis J, Mikuls TR, Cerhan JR, Criswell LA, Saag KG; Iowa Women’s Health Study. Vitamin D intake is inversely associated with rheumatoid arthritis: results from the Iowa Women’s Health Study. Arthritis Rheum. 2004 Jan;50(1):72-7. doi: 10.1002/art.11434.
Messa P, Curreri M, Regalia A, Alfieri CM. Vitamin D and the cardiovascular system: an overview of the recent literature. Am J Cardiovasc Drugs. 2014 Feb;14(1):1-14. doi: 10.1007/s40256-013-0047-y.
Murdaca G, Gerosa A, Paladin F, Petrocchi L, Banchero S, Gangemi S. Vitamin D and Microbiota: Is There a Link with Allergies? Int J Mol Sci. 2021 Apr 20;22(8):4288. doi: 10.3390/ijms22084288.
Ombra MN, Paliogiannis P, Doneddu V, Sini MC, Colombino M, Rozzo C, Stanganelli I, Tanda F, Cossu A, Palmieri G. Vitamin D status and risk for malignant cutaneous melanoma: recent advances. Eur J Cancer Prev. 2017 Nov;26(6):532-541. doi: 10.1097/CEJ.0000000000000334.
Pérez-López FR, Pasupuleti V, Mezones-Holguin E, Benites-Zapata VA, Thota P, Deshpande A, Hernandez AV. Effect of vitamin D supplementation during pregnancy on maternal and neonatal outcomes: a systematic review and meta-analysis of randomized controlled trials. Fertil Steril. 2015 May;103(5):1278-88.e4. doi: 10.1016/j.fertnstert.2015.02.019.
Poel YH, Hummel P, Lips P, Stam F, van der Ploeg T, Simsek S. Vitamin D and gestational diabetes: a systematic review and meta-analysis. Eur J Intern Med. 2012 Jul;23(5):465-9. doi: 10.1016/j.ejim.2012.01.007.
Reid IR, Bolland MJ, Grey A. Effects of vitamin D supplements on bone mineral density: a systematic review and meta-analysis. Lancet. 2014 Jan 11;383(9912):146-55. doi: 10.1016/S0140-6736(13)61647-5.
Rose AA, Elser C, Ennis M, Goodwin PJ. Blood levels of vitamin D and early stage breast cancer prognosis: a systematic review and meta-analysis. Breast Cancer Res Treat. 2013 Oct;141(3):331-9. doi: 10.1007/s10549-013-2713-9.
Sadeghian M, Saneei P, Siassi F, Esmaillzadeh A. Vitamin D status in relation to Crohn’s disease: Meta-analysis of observational studies. Nutrition. 2016 May;32(5):505-14. doi: 10.1016/j.nut.2015.11.008.
Salehpour A, Hosseinpanah F, Shidfar F, Vafa M, Razaghi M, Dehghani S, Hoshiarrad A, Gohari M. A 12-week double-blind randomized clinical trial of vitamin D₃ supplementation on body fat mass in healthy overweight and obese women. Nutr J. 2012 Sep 22;11:78. doi: 10.1186/1475-2891-11-78.
Shen L, Ji HF. Vitamin D deficiency is associated with increased risk of Alzheimer’s disease and dementia: evidence from meta-analysis. Nutr J. 2015 Aug 1;14:76. doi: 10.1186/s12937-015-0063-7.
Sigmund CD. Regulation of renin expression and blood pressure by vitamin D(3). J Clin Invest. 2002 Jul;110(2):155-6. doi: 10.1172/JCI16160.
Sørensen IM, Joner G, Jenum PA, Eskild A, Torjesen PA, Stene LC. Maternal serum levels of 25-hydroxy-vitamin D during pregnancy and risk of type 1 diabetes in the offspring. Diabetes. 2012 Jan;61(1):175-8. doi: 10.2337/db11-0875.
Sperati F, Vici P, Maugeri-Saccà M, Stranges S, Santesso N, Mariani L, Giordano A, Sergi D, Pizzuti L, Di Lauro L, Montella M, Crispo A, Mottolese M, Barba M. Vitamin D supplementation and breast cancer prevention: a systematic review and meta-analysis of randomized clinical trials. PLoS One. 2013 Jul 22;8(7):e69269. doi: 10.1371/journal.pone.0069269.
Staples J, Ponsonby AL, Lim L. Low maternal exposure to ultraviolet radiation in pregnancy, month of birth, and risk of multiple sclerosis in offspring: longitudinal analysis. BMJ. 2010 Apr 29;340:c1640. doi: 10.1136/bmj.c1640. PMID: 21030361; PMCID: PMC2862149.
Sutton AL, MacDonald PN. Vitamin D: more than a “bone-a-fide” hormone. Mol Endocrinol. 2003 May;17(5):777-91. doi: 10.1210/me.2002-0363.
Thomas GN, ó Hartaigh B, Bosch JA, Pilz S, Loerbroks A, Kleber ME, Fischer JE, Grammer TB, Böhm BO, März W. Vitamin D levels predict all-cause and cardiovascular disease mortality in subjects with the metabolic syndrome: the Ludwigshafen Risk and Cardiovascular Health (LURIC) Study. Diabetes Care. 2012 May;35(5):1158-64. doi: 10.2337/dc11-1714.
Thorne J, Campbell MJ. The vitamin D receptor in cancer. Proc Nutr Soc. 2008 May;67(2):115-27. doi: 10.1017/S0029665108006964.
Timerman D, McEnery-Stonelake M, Joyce CJ, Nambudiri VE, Hodi FS, Claus EB, Ibrahim N, Lin JY. Vitamin D deficiency is associated with a worse prognosis in metastatic melanoma. Oncotarget. 2017 Jan 24;8(4):6873-6882. doi: 10.18632/oncotarget.14316.
Vahdaninia M, Mackenzie H, Helps S, Dean T. Prenatal Intake of Vitamins and Allergic Outcomes in the Offspring: A Systematic Review and Meta-Analysis. J Allergy Clin Immunol Pract. 2017 May-Jun;5(3):771-778.e5. doi: 10.1016/j.jaip.2016.09.024.
Wacker M, Holick MF. Vitamin D – effects on skeletal and extraskeletal health and the need for supplementation. Nutrients. 2013 Jan 10;5(1):111-48. doi: 10.3390/nu5010111.
Wang D, Vélez de-la-Paz OI, Zhai JX, Liu DW. Serum 25-hydroxyvitamin D and breast cancer risk: a meta-analysis of prospective studies. Tumour Biol. 2013 Dec;34(6):3509-17. doi: 10.1007/s13277-013-0929-2.
Wei SQ, Qi HP, Luo ZC, Fraser WD. Maternal vitamin D status and adverse pregnancy outcomes: a systematic review and meta-analysis. J Matern Fetal Neonatal Med. 2013 Jun;26(9):889-99. doi: 10.3109/14767058.2013.765849.
Xu Y, Shao X, Yao Y, Xu L, Chang L, Jiang Z, Lin Z. Positive association between circulating 25-hydroxyvitamin D levels and prostate cancer risk: new findings from an updated meta-analysis. J Cancer Res Clin Oncol. 2014 Sep;140(9):1465-77. doi: 10.1007/s00432-014-1706-3.
Yin L, Ordóñez-Mena JM, Chen T, Schöttker B, Arndt V, Brenner H. Circulating 25-hydroxyvitamin D serum concentration and total cancer incidence and mortality: a systematic review and meta-analysis. Prev Med. 2013 Dec;57(6):753-64. doi: 10.1016/j.ypmed.2013.08.026.
Zhang H, Zhang H, Wen X, Zhang Y, Wei X, Liu T. Vitamin D Deficiency and Increased Risk of Bladder Carcinoma: A Meta-Analysis. Cell Physiol Biochem. 2015;37(5):1686-92. doi: 10.1159/000438534.
Zhang L, Wang S, Che X, Li X. Vitamin D and lung cancer risk: a comprehensive review and meta-analysis. Cell Physiol Biochem. 2015;36(1):299-305. doi: 10.1159/000374072.
Zhang MX, Pan GT, Guo JF, Li BY, Qin LQ, Zhang ZL. Vitamin D Deficiency Increases the Risk of Gestational Diabetes Mellitus: A Meta-Analysis of Observational Studies. Nutrients. 2015 Oct 1;7(10):8366-75. doi: 10.3390/nu7105398.
Zhao Y, Sun Y, Ji HF, Shen L. Vitamin D levels in Alzheimer’s and Parkinson’s diseases: a meta-analysis. Nutrition. 2013 Jun;29(6):828-32. doi: 10.1016/j.nut.2012.11.018.